0618
Sodium accumulation in primary motor areas, an early feature of amyotrophic lateral sclerosis patients1Aix-Marseille Univ, CNRS, CRMBM, Marseille, France, 2Aix-Marseille Univ, APHM, Hopital de la Timone, ALS department, Marseille, France, 3Aix-Marseille Univ, APHM, Hopital de la Timone, CEMEREM, Marseille, France
Synopsis
Amyotrophic lateral sclerosis (ALS) is a rapidly fatal neurodegenerative disease characterized by upper (in brain) and lower (in spine) motor neuron degeneration. As conventional MRI fails to show brain motor neurons impairment in ALS, advanced techniques are needed to improve the diagnosis and to monitor the progression of the disease. In this study, brain 23Na MRI was applied in 15 ALS patients and 31 controls. A common pattern of sodium accumulation was found in patients in the primary motor areas while no atrophy was detected. The occurrence of sodium accumulation without atrophy probably reflects early neuronal injury in ALS.
BACKGROUND
Amyotrophic lateral sclerosis (ALS) is a lethal neurodegenerative disease that induces a death of upper (in brain) and lower (in spine) motor neurons. To date, diagnosis and management of ALS is only based on clinical and electrophysiological exploration. A high variability is seen in patient presentation and evolution, with a survival delay from few months to a decade. Even if central nervous system (CNS) is involved in ALS, conventional MRI fails to show brain abnormalities. Thus, to depict the CNS impairment in ALS, advanced MRI techniques are required. Brain sodium MRI, a technique that previously showed its ability to detect neuronal dysfunction1,2,3 seems to be of major interest in ALS.PURPOSE
To evaluate brain neuronal impairment in ALS patients using 23Na MRI.METHODS
MR scans were performed on a 3T Verio system (Siemens, Germany) in 15 ALS patients (6F/9M; mean age 56±9 yo; mean disease duration 13±17 months) and 31 healthy controls (16F/15M, mean age 45±13 yo). ALS patients had a clinical and electrophysiological evaluation the same day as the MRI. 23Na MRI was acquired using a double-tuned 23Na-1H volume head coil (RapidBiomedical, Germany) and a 3D density-adapted radial projection reconstruction pulse sequence4 (TE=200μs/TR=120ms, 17000 projections and 369 samples per projection, 3.6mm3 isotropic resolution, acquisition time = 34min) with two tubes filled with 50 mM of sodium placed in the FOV to serve for external references. High-resolution proton MRI 3D-MPRAGE (TR=2300ms/TE=3ms/TI=900ms, 160 slices, 1mm3 isotropic resolution) was obtained using a 32-element 1H head coil (Siemens). The optimized post-processing pipeline is described in Figure 1. A voxel-based statistical mapping analysis (SPM8) was conducted onto the spatially normalized and smoothed quantitative sodium concentration maps of all subjects to compare at the voxelwise level the total sodium concentration (TSC) between ALS patients and healthy controls (SPM8, p<0.005, FWE corrected). In order to evaluate the contribution of brain atrophy on abnormal TSC clusters, we performed an overlay of abnormal TSC maps with grey matter (GM) atrophy maps that were generated by a voxel-based statistical mapping analysis performed on the normalized and smoothed GM density maps, resulting from the segmentation of 3D-MPRAGE (SPM8, T-test patients vs controls, p<0.005, FWE corrected).RESULTS
The voxel-based analysis evidenced the presence of brain sodium accumulation in ALS patients as shown in Figure 2 (T-test, p<0.005, FWE corrected). These sodium accumulations were located in specific regions namely the primary motor areas and the corpus callosum (Figure 2). As mentioned in Figure 3, the total sodium concentration within these abnormal clusters was significantly higher in ALS patients compared to controls (p=0.0004). Conventional 1H MRI was normal in patients, as commonly seen in ALS. Comparison of sodium accumulation and GM atrophy showed that sodium accumulation did not co-locate with GM atrophy in ALS patients (Figure 4).DISCUSSION
This first sodium MRI study in ALS evidenced the presence of brain sodium accumulation in ALS patients. Despite the clinical heterogeneity of ALS patients, we found a common pattern of the topography of sodium accumulation that was located in the primary motor area. This location is in accordance with the pathophysiology of the disease affecting upper motor neurons. Interestingly, sodium accumulation did not co-locate with GM atrophy. As neuronal loss is commonly reflected by atrophy, the occurrence of sodium accumulation without atrophy suggests that sodium accumulation can be an earlier marker of neuronal injury.Acknowledgements
This research is funded by APHM (Assistance Publique des Hôpitaux de Marseille)References
(1) Shah NJ, Worthoff WA, Langen KJ. Imaging of sodium in the brain: a brief review. NMR Biomed. 2016 Feb;29(2):162-74.
(2) Maarouf A, Audoin B, Konstandin S et al. Topography of brain sodium accumulation in progressive multiple sclerosis. MAGMA. 2014; 27(1):53-62.
(3) Zaaraoui W, Konstandin S, Audoin B at al. Distribution of brain sodium accumulation correlates with disability in multiple sclerosis: a Cross-sectional 23Na MR Imaging Study. Radiology. 2012; 264(3):859-67.
(4) Nagel AM, Laun FB, Weber MA, et al. Sodium MRI using a density-adapted 3D radial acquisition technique. Magn Reson Med. 2009; 62(6):1565-73.
Figures
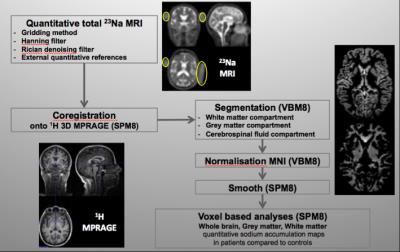
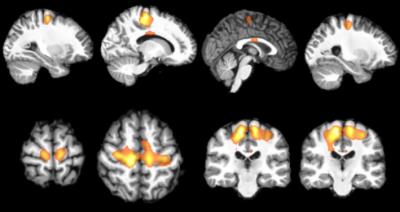
Figure 2: Topography of brain sodium accumulation in ALS patients
(SPM8, T-test patients vs controls, p<0.005, FWE corrected)
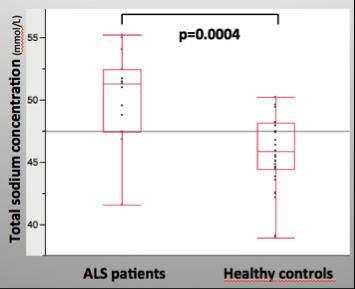
Figure 3: Comparison between ALS patients and healthy controls of sodium concentration extracted from the cluster of sodium accumulation in patients
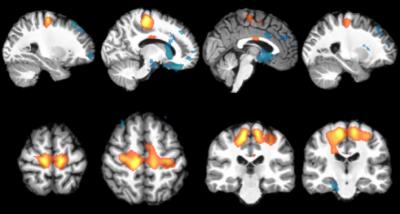
Figure 4: Topography of brain sodium accumulation (orange) and grey matter atrophy (blue) in ALS patients compared to controls
(SPM8, T-test patients vs controls, p<0.005, FWE corrected)