0537
Detection of Internal Tissue Disruptions within the Intervertebral Disc via Magnetic Resonance Elastography: A Feasibility StudyBenjamin A Walter1,2, Prasath Mageswaran1,3, Elizabeth Yu1,4, Safdar Khan1,4, William S Marras1,3, and Arunark Kolipaka1,5
1Spine Research Institute, The Ohio State University, Columbus, OH, United States, 2Department of Biomedical Engineering, The Ohio State University, Columbus, OH, United States, 3Department of Integrated Systems Engineering, The Ohio State University, Columbus, OH, United States, 4Department of Orthopaedics, The Ohio State University Wexner Medical Center, Columbus, OH, United States, 5Department of Radiology, The Ohio State University Wexner Medical Center, Columbus, OH, United States
Synopsis
Magnetic resonance elastography (MRE) was used to non-invasively assess regions of internal tissue disruption within intervertebral discs (IVD) that were known to contain tissue damage. Internal tissue disruptions were assessed via measurements of wave continuity as they propagated throughout the IVD. Results demonstrated that injured IVD’s had an elevated octahedral shear strain (OSS) compared to non-operated control IVDs and OSS maps allowed visualization of potential location of internal tissue disruptions. Overall, results of this study suggest that MRE may provide a non-invasive way of identifying internal tissue disruptions within the IVD.
Purpose:
Low back pain is the leading cause of disability worldwide [1], however, diagnosing the cause/source of pain is a significant clinical challenge. The development of internal disruptions within the intervertebral disc (IVD), such as annular fissures, is significantly associated with the development of low back pain [2, 3] and can promote tissue instability and create a permissive environment for nerve ingrowth. However, currently the only clinical means of confirming whether an IVD contains internal disruptions is via a procedure (i.e., provocative discography) that has become highly controversial due to its invasive nature the resultant increase in future risk of clinical problems [4]. Therefore, this study aimed to determine if magnetic resonance elastography (MRE) could be used as a non-invasive alternative to identify internal disruptions present within the IVD.Methods:
Patients who either had a disc herniation but had not yet undergone surgery (n=1) or had previously undergone a micro-discectomy (n=3) were scanned. Surgical patients were chosen to ensure that at least one IVD contained existing tissue damage. All protocols were approved by The Ohio State University institutional review board and all images were acquired on a 3T MRI scanner (Trim Trio, Siemens). A sagittal T2 weighted image of the lumbar spine was collected for overall assessment of the lumbar spine. A T2 weighted transverse image of each IVD was acquired immediately prior to the application of a standard gradient recalled echo (GRE) MRE sequence which was used to acquire a single two-dimensional (2D) transverse slice through each IVD (slice thickness=5mm). All lumbar levels with sufficient disc height were collected. Mechanical vibrations were applied to the subjects lower back via a pneumatic driver system and the in- and through- plane displacements were encoded. To assess the wave continuity throughout each IVD, the phase data of each phase offset was analyzed via a octahedral shear strain analysis [5,6] modified for a single slice. OSS is a single value that represents the maximum shear strain occurring at a point across all possible planes and can therefore quantify the degree of shear displacement discontinuity within the tissue. If there is a fissure or crack within the tissue the wave propagation will be scattered once it encounters the internal discontinuity thereby allowing the creation of an OSS map that may allow visualization of an internal crack. In addition to the generation of OSS maps for each IVD the whole IVD was traced by hand and the central nucleus pulposus (NP) region was determined using a custom MATLAB code. The average OSS value within the NP region was compared between the injured IVD and the average of “healthy” un-operated controls within the same patient.Results:
In three of the four subjects the IVDs that were either operated on or had a herniation had a greater average OSS than the non-operated/non-injured controls (Figure 1). The OSS maps of the operated discs from two of the three patients demonstrated clear regions of wave discontinuity that originates in the annulus fibrosus and continues into the NP region (Figure 2). The three herniated IVDs also demonstrated a high OSS strain in the circumferential direction originating near the posterior herniation (Figure 3) suggesting possible circumferential tears.Discussion:
This pilot study demonstrated that OSS analysis was able to differentiate between injured IVDs (damaged via herniation or surgery) and control IVDs and that OSS maps allowed visualization of the likely area surgical path. These results suggest that MRE can be used to non-invasively assess IVD tissue continuity. The variability seen in the OSS maps between operated IVDs is likely influenced by the degree of surgical penetration into the IVD during the procedure which can vary from only removal of the herniated tissue fragment to also removing NP tissue further within the IVD to prevent future re-herniation. While further work is required to determine if MRE can detect smaller injuries and if MRE-detected tissue disruptions are associated with pain, this study demonstrates the feasibility of MRE to identify internal tissue disruption without the use of provocative discography. Given the controversy regarding provocative discography, MRE may provide a non-invasive tool to aid clinical treatment of low back pain that does not promote future clinical problems.Conclusion:
This study demonstrates that MRE can be used to identify internal tissue disruptions within the IVD.Acknowledgements
This work was funded by NIH R01HL124096 and the Spine Research Institute at The Ohio State University.References
[1] Vos+ Lancet 2012 [2] Bogduk+ Pain Med 2013 [3] Videman+ Spin 2004 [4] Carragee+ Spine 2016 [5] McGarry+ Phys Med Biol 2011 [6] Papazoglou+ Phys Med Biol 2007Figures
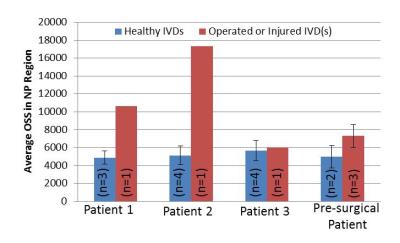
Figure 1: Average Octahedral Shear Strain within
the nucleus pulposus region of injured and non-injured IVDs. N refers to the number of IVDs from that
patient.
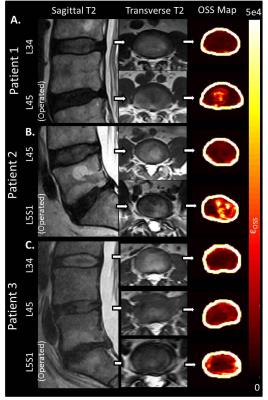
Figure 2: Octahedral Shear Strain Maps on IVDs
from patients who have undergone a micro-discectomy. High OSS represents an
area of high tissue discontinuity.
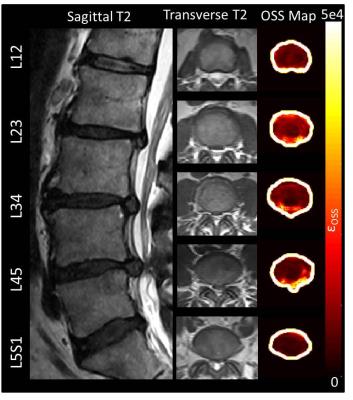
Figure 3: Octahedral Shear Strain Maps on IVDs from a
patient with IVD herniation. High OSS in
the circumferential direction on herniated IVDs suggests the presence of
circumferential fissures in addition to a herniation.