0434
The value of high resolution gadoextic acid-enhanced MR cholangiography for evaluating biliary anatomy of living liver donor: comparison with T2 weighted (T2W) MR cholangiography and conventional gadoxetic acid enhanced MR cholangiography1Radiology, Seoul National University Hospital, Seoul, Korea, Republic of
Synopsis
The addition of gadoxetic acid-enhanced sFOV T1W-MRC to T2W-MRC is able to provide more precise depiction of biliary anatomy, which is crucial for the prevention of post-operative biliary complications of living liver donors.
Introduction
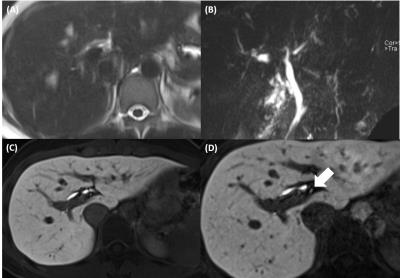
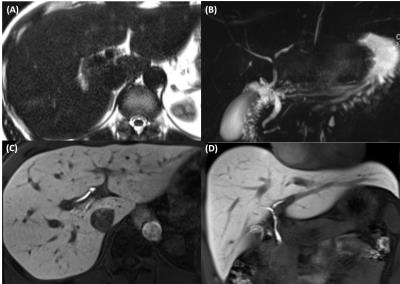
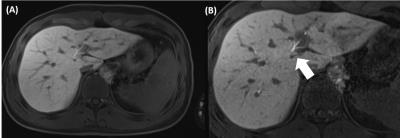
The precise assessment of biliary anatomy is crucial for guiding for surgical approach and preventing complication, which is most common postoperative complication of living liver donor transplantation.1-3Among various methods to evaluate biliary anatomy of donor, MR cholangiography (MRC) has a strength in terms of non-invasiveness, no radiation hazard and low risk of hypersensitivity reaction.4,5 However, the conventional T2-weighted (T2W) MRC is often in conclusive due to poor spatial resolution or severe motion artifacts, and/or limited signal to noise ratio.6-10 Also, conventional gadoxetic acid enhanced T1-weighted (T1W) MRC has marginal spatial resolution for assessment of intrahepatic bile duct, although it may provide higher spatial resolution than T2W MRC.11,12 So, to make breakthrough of those limitation of MRC, we attempted to determine the incremental value of small field of view (sFOV), high resolution, gadoxetic acid-enhanced T1W-MRC for the evaluation of the biliary anatomy of potential living donors, compared to T2W-MRC.Methods
73 living donors were examined with gadoxetic acid-enhanced MRI including 3 kinds of MRCs: a) three-dimensional (3D) multislice T2W-MRC; b) regular FOV (rFOV) (320~380mm) 3D T1W-MRC with a slice thickness (ST) of 3mm, acceleration factor, 2X2; phase oversampling rate 13%; and c) sFOV (256x208mm) T1W-MRC with a ST of 1 mm, acceleration factor 2x2, phase oversampling rate 26%. Three radiologists reviewed three image sets in terms of visibility of segmental intrahepatic bile ducts (BD), biliary anatomy, and expected BD opening number on right hemihepatectomy: 1) T2W-MRC alone, 2) T2W-MRC with rFOV T1W-MRC, and 3) T2W-MRC with sFOV T1W-MRC. They scored BD visibility scores in a 4-point scale, visible BD level in a 5-point scale, and also scored their confidence level for biliary anatomy in a 4-point scale. Analysis of variance, χ2-test, and interobserver agreement were used to determine statistically significant differences between the three imaging sets.Results
When sFOV T1W-MRC was added to T2W-MRC, BD visibility score (average, 3.16 ± 0.63 vs. 3.36 ± 0.51; P <.01), visible BD level (average, 4.18 ± 0.16 vs. 4.51 ± 0.39; P <.01) and confidence levels for biliary anatomy (average 3.33 ± 0.33 vs. 3.86 ± 0.28; P<.01) were significantly improved compared to T2W-MRC alone. Interobserver agreement for predicting biliary anatomy was also better in sFOV T1W-MRC with T2W-MRC set than in T2W-MRC alone (к value; 0.60~0.64 vs 0.66~0.81). Furthermore, compared with the rFOV T1W-MRC set, segment 1 BD visibility was significantly increased (average, 52.9% (116/219) vs 69.9% (153/219); P<.001). Among patients in whom T2W-MRC presented sub-diagnostic image quality, the addition of sFOV T1W-MRC provided diagnostically acceptable image visibility in 77.2% (17/22) for reviewer 1, 53.8% (14/26) for reviewer 2, and 90% (18/20) for reviewer 3. For determination of BD opening number, addition of sFOV T1W-MRC to T2W-MRC (68.5%, k=0.48) provided higher consistency and agreement with surgical findings than T2W-MRC alone (65.8%, k=0.43) but fail to meet statistical significance (p=0.306).Discussion
The addition of sFOV T1W-MRC to T2W-MRC significantly improved BD visibility and confidence levels for biliary anatomy compared with T2W-MRC alone, allowing proper biliary anatomy assessment in most cases of sub-diagnostic T2W-MRC. Also, substitution rFOV T1W-MRC to sFOV T1W-MRC showed higher BD visibility, especially in B1 with statistical significance.Conclusion
The addition of gadoxetic acid-enhanced sFOV T1W-MRC to T2W-MRC is able to provide more precise depiction of biliary anatomy, which is crucial for the prevention of post-operative biliary complications of living liver donors.Acknowledgements
No acknowledgement found.References
1. Welling TH, Heidt DG, Englesbe MJ, et al. Biliary complications following liver transplantation in the model for end-stage liver disease era: Effect of donor, recipient, and technical factors. Liver Transplantation 2008;14(1):73-80.
2. Hwang S, Lee SG, Sung KB, et al. Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver transplantation 2006;12(5):831-838.
3. Wadhawan M, Kumar A, Gupta S, et al. Post-transplant biliary complications: An analysis from a predominantly living donor liver transplant center. Journal of gastroenterology and hepatology 2013;28(6):1056-1060.
4. Persson A, Dahlstrom N, Smedby O, Brismar TB. Three-dimensional drip infusion CT cholangiography in patients with suspected obstructive biliary disease: a retrospective analysis of feasibility and adverse reaction to contrast material. BMC Med Imaging 2006;6:1.
5. Schroeder T, Radtke A, Kuehl H, Debatin JF, Malago M, Ruehm SG. Evaluation of living liver donors with an all-inclusive 3D multi-detector row CT protocol. Radiology 2006;238(3):900-910.
6. Fulcher AS, Szucs RA, Bassignani MJ, Marcos A. Right lobe living donor liver transplantation: preoperative evaluation of the donor with MR imaging. American Journal of Roentgenology 2001;176(6):1483-1491.
7. An SK, Lee JM, Suh K-S, et al. Gadobenate dimeglumine-enhanced liver MRI as the sole preoperative imaging technique: a prospective study of living liver donors. American Journal of Roentgenology 2006;187(5):1223-1233.
8. Fulcher AS, Turner MA, Franklin KJ, et al. Primary Sclerosing Cholangitis: Evaluation with MR Cholangiography—A Case-Control Study 1. Radiology 2000;215(1):71-80.
9. Kaltenthaler EC, Walters SJ, Chilcott J, Blakeborough A, Vergel YB, Thomas S. MRCP compared to diagnostic ERCP for diagnosis when biliary obstruction is suspected: a systematic review. BMC medical imaging 2006;6(1):1.
10. Rösch T, Meining A, Frühmorgen S, et al. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointestinal endoscopy 2002;55(7):870-876.
11. Lee ES, Lee JM, Yu MH, et al. High spatial resolution, respiratory-gated, t1-weighted magnetic resonance imaging of the liver and the biliary tract during the hepatobiliary phase of gadoxetic Acid-enhanced magnetic resonance imaging. J Comput Assist Tomogr 2014;38(3):360-366.
12. Yoon JH, Lee JM, Lee ES, et al. Navigated three-dimensional T1-weighted gradient-echo sequence for gadoxetic acid liver magnetic resonance imaging in patients with limited breath-holding capacity. Abdom Imaging 2015;40(2):278-288.
Figures