0341
Association between Age of Intraplaque Hemorrhage and Fibrous Cap Rupture in Carotid Artery Atherosclerosis: A High Resolution Magnetic Resonance Imaging Study1Department of Radiology, The General Hospital of People’s Liberation Army (301 hospital), Beijing, People's Republic of China, 2Center for Biomedical Imaging Research, Department of Biomedical Engineering, Tsinghua University, Beijing, People's Republic of China, 3Department of Radiology, University of Washington, Seattle, United States, 4Beijing Institute for Brain Disorders, Capital Medical University, Beijing, People's Republic of China
Synopsis
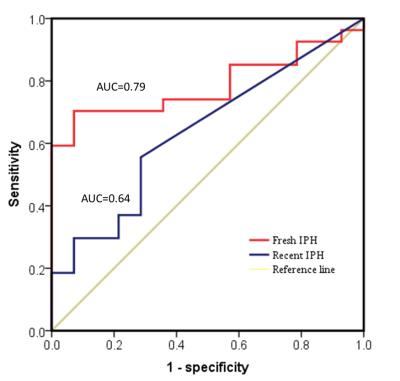
It has been shown that presence of carotid artery intraplaque hemorrhage (IPH) is associated with fibrous cap rupture (FCR), which is one of the major causes of ischemic cerebrovascular events. However, the role of different age of IPH in occurrence of IPH remains unclear. This study investigated the association between the age of IPH and FCR in carotid arteries using MR imaging. We found that fresh IPH volume was independently associated with FCR (odds ratio: 1.826; 95% CI: 1.130-2.949; P=0.014). Compared with recent IPH, fresh IPH was a stronger predictor for FCR (area under the curve: 0.79 vs. 0.64).
Introduction and Purpose
Fibrous cap rupture (FCR) of carotid atherosclerotic plaque is associated with ischemic cerebrovascular events [1]. Intrapalque hemorrhage (IPH), as one of the vulnerable plaque features, has been demonstrated to be a strong predictor for carotid FCR [2,3]. Histologically, the components of IPH vary with the evolution of erythrocytic metabolins. A previous MR imaging study has shown that IPH can be classified into fresh and recent stages according to the time of bleeding [4]. However, it is unclear that if the different age of IPH plays different role in plaque vulnerability, particularly the occurrence of FCR. In this study, we sought to investigate the association between the age of IPH and FCR in carotid arteries by using multi-contrast magnetic resource (MR) vessel wall imaging.Methods
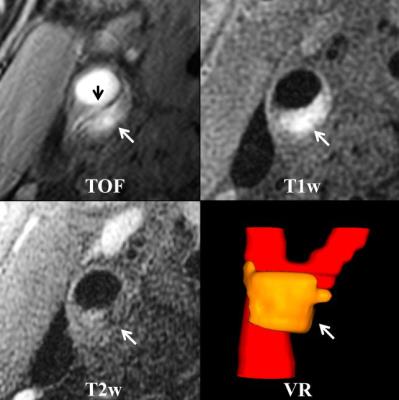
Study sample: Patients with cerebrovascular symptoms and carotid atherosclerotic plaque determined by ultrasound were recruited and underwent carotid artery MR vessel wall imaging. Carotid arteries with IPH on MR images were eligible for data analysis and those with ulceration, occlusion or incomplete coverage for IPH were excluded. MR imaging: The MR imaging was performed on a GE 3.0 T MR scanner with a 4-channel carotid coil. A multi-contrast MR imaging protocol including 3D time-of-flight (TOF), 2D T1-weighted (T1w) and T2-weighted (T2w) imaging was acquired with the following parameters: 3D TOF: gradient echo, TR/TE 29/2.1 ms, and flip angle 20º; T1w: black-blood fast spin echo (FSE), TR/TE 800/8.9 ms, and flip angle 90º; T2w: black-blood FSE, TR/TE 3000/57 ms and flip angle 90º. All imaging sequences were scanned with the same FOV (140x140 mm2), matrix size (256x256), and slice thickness (2 mm). Data analysis: Two experienced radiologists interpreted the MR images using custom-designed software ‘CASCADE’ with consensus. The FCR was defined as non-ulcerated fissured fibrous cap. The age of IPH including fresh and recent stage was evaluated and stenosis was measured. The association between age of IPH and presence of FCR was determined. Institutional review board approval and informed consent were obtained.Results
In total, 41 carotid arteries in 37 patients (mean age 70.2±11.0 years old; 32 males) were eligible for final statistics analysis. Mann-Whitney ranks analysis revealed that fresh IPH volume in plaques with FCR was significantly larger than that of those without FCR (48.7±36.1 mm3 vs.14.2±9.6 mm3, P=0.003). In contrast, significant difference was not found in recent IPH volume between plaques with and without FCR (19.6±38.5 mm3 vs. 5.1±10.9 mm3, P=0.120). Logistic regression showed that the odds ratio (OR) of fresh IPH volume and recent IPH volume was 1.828 (95% confidence interval [CI], 1.147-2.912, P=0.011), 1.392 (95% CI, 0.846-2.290, P=0.193) in discriminating presence of FCR, respectively. In predicting presence of FCR, the OR of fresh IPH volume and recent IPH volume was 1.826 (95% CI, 1.130-2.949, P=0.014) and 1.479 (95% CI 0.865-2.528, P=0.153) after adjusting confounding factors, respectively. Receiver operating character (ROC) analysis showed, in discriminating presence of FCR, fresh IPH volume had higher area-under-the-curve (AUC) (AUC=0.79, 95% CI 0.65-0.93) compared to recent IPH volume (AUC=0.64, 95% CI 0.46-0.81) (Figure 1). Figure 2 is an example showing the occurrence of FCR in a carotid plaque with fresh IPH.Discussion
This study investigated the association between the age of IPH and FCR using MR imaging. We found that fresh IPH volume was independently associated with FCR. Compared with recent IPH, fresh IPH was a stronger predictor for FCR. In the acute phase of IPH, leukocytes, particularly neutrophils, and plasma zymogen, were conveyed in plaque with the red blood cell entrance. These two components of acute IPH were the key sources of proteases, which account for a major part of the proteolytic degradation of fibrous cap[5,6]. The increases of the size and complexity of the plaque due to IPH will subsequently increase the amount of activated proteases within plaque [7]. Besides, IPH had a close correlation with enhanced stress over fibrous cap [8,9]. It was reported that the stress over fibrous cap is decreasing during the acute phase of IPH by 30% from 159 kPa (114-253) to 118 kPa (79-189) [10].Conclusion
Fresh intraplaque hemorrhage volume is independently associated with presence of fibrous cap rupture in carotid atherosclerotic plaques, suggesting the age of IPH might be an effective indicator for plaque disruption.Acknowledgements
NoneReferences
1. Gupta A, Baradaran H, Schweitzer AD, et al. Carotid plaque MRI and stroke risk: a systematic review and meta-analysis. Stroke. 2013;44:3071-7.
2. van Dijk AC, Truijman MT, Hussain B, et al. Intraplaque hemorrhage and the plaque surface in carotid atherosclerosis: The plaque at risk study (PARISK). AJNR Am J Neuroradiol. 2015;36:2127-33.
3. Treiman J, McNally S, Parker D, et al. Correlation of carotid intraplaque hemorrhage and stroke using 1.5 T and 3 T MRI. Magn Reson Insights. 2015;8:1-8.
4. Chu B, Kampschulte A, Ferguson MS, et al. Hemorrhage in the atherosclerotic carotid plaque: a high-resolution MRI study. Stroke. 2004;35:1079-84.
5. Michel J B, Delbosc S, Ho-Tin-Noe B, et al. From intraplaque haemorrhages to plaque vulnerability: biological consequences of intraplaque haemorrhages. J Cardiovasc Med (Hagerstown). 2012;13:628-34.
6. Michel J B, Virmani R, Arbustini E, et al. Intraplaque haemorrhages as the trigger of plaque vulnerability. Eur Heart J. 2011;32:1977-85,85a,85b,85c.
7. Leclercq A, Houard X, Loyau S, et al. Topology of protease activities reflects atherothrombotic plaque complexity. Atherosclerosis. 2007;191:1-10.
8. Sadat U, Teng Z, Young VE, et al. Utility of magnetic resonance imaging-based finite element analysis for the biomechanical stress analysis of hemorrhagic and non-hemorrhagic carotid plaques. Circ J. 2011;75:884-9.
9. Huang X, Teng Z, Canton G, et al. Intraplaque hemorrhage is associated with higher structural stresses in human atherosclerotic plaques: an in vivo MRI-based 3D fluid-structure interaction study. Biomed Eng Online. 2010;9:86.
10. Sadat U, Teng Z, Young VE, et al. Impact of plaque haemorrhage and its age on structural stresses in atherosclerotic plaques of patients with carotid artery disease: an MR imaging-based finite element simulation study. Int J Cardiovasc Imaging. 2011;27:397-402.
Figures