0340
Association between Carotid Atherosclerotic Plaque Calcification and Intraplaque Hemorrhage: A High Resolution Magnetic Resonance Imaging Study1Center for Biomedical Imaging Research, Department of Biomedical Engineering, School of Medicine, Tsinghua University, Beijing, People's Republic of China, 2Department of Radiology, Fujian Union Hospital, People's Republic of China, 3Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, People's Republic of China
Synopsis
Carotid intraplaque hemorrhage (IPH) is associated with cardiovascular events. Calcification, frequently accompanied with IPH, may play a role in occurrence of IPH. In this study we aimed to investigate the associations between calcification characteristics and IPH in carotid plaques. Our results suggest that surface calcification and multiple calcification in carotid atherosclerotic plaques are independently associated with presence IPH. Both quantity and location of calcification may play important roles in occurrence of IPH. These findings may provide novel insights for understanding the mechanism of IPH.
Introduction
Intraplaque hemorrhage (IPH) play the key role in plaque vulnerability and plaque progression [1]. However, the pathogenesis of IPH is still unclear. Most of the investigators believe that the rupture of immature neovessel might be the pathological basis [2,3]. There is a hypothesis that the interaction between neovessel and other intraplaque compositional features, particularly calcification, may play a role in occurrence of IPH [4-6]. However, few studies have been performed to investigate the relationships between calcification charateristics and IPH.Purpose
The purpose of this study was to determine the associations between IPH and calcification characteristics, such as quantity and location, in carotid atherosclerotic plaques using high-resolution magnetic resonance imaging (HRMRI) in vivo.Methods
Study population
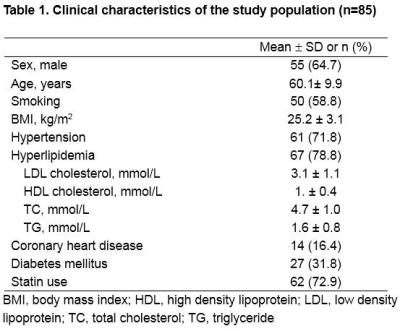
Eighty-five patients with recent ischemic stroke or TIA (within 2 weeks) and carotid artery atherosclerotic plaque determined by ultrasound were recruited. All patients underwent MR imaging for bilateral carotid arteries. The clinical information was also recorded.
Carotid MR imaging and Image interpretation
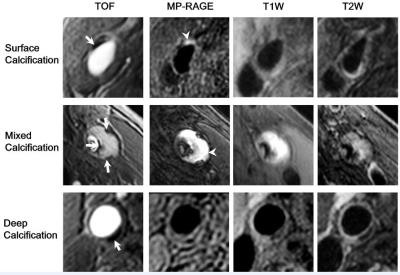
Carotid MR imaging was performed on a whole body 3.0-Tesla MR scanner (Achieva TX, Philips, the Netherlands) with a custom-designed 36-channel neurovascular coil [7]. The carotid arteries were imaged using a multicontrast vessel wall imaging protocol (3D-TOF, T1W-QIR, T2W-MDIR, MP-RAGE). All carotid MR images were interpreted by two radiologists with more than 5 years’ experience blinded to clinical information using a custom-designed software of CASCADE [8]. Only plaques with composition such as calcification, lipid-rich necrotic core, or IPH, were further studied. The location of the calcification was graded with the following categories: surface calcification; mixed calcification (both surface and deep calcification are present), and deep calcification. The calcification was also classified into single and multiple calcifications. The wall thickness for each plaque was measured.
Statistical analysis
Continuous quantitative variables are described as mean±SD and the percentage is used to describe the categorical variables. The characteristics of clinical information and carotid calcifications between patients with and without carotid IPH were compared. Generalized estimating equations were used to eliminate the correlation between plaques in bilateral carotid arteries in the same participant. Logistic regression models were used to calculate the odds ratio (OR) and corresponding 95% confidence interval (CI) of characteristics of calcification in discriminating presence of carotid IPH. Univariate regression analysis and multivariate regression models were utilized to adjust for potential confounding factors. All statistical analysis was performed with SAS software version 9.4 (SAS Institute Inc, Cary, NC).
Results
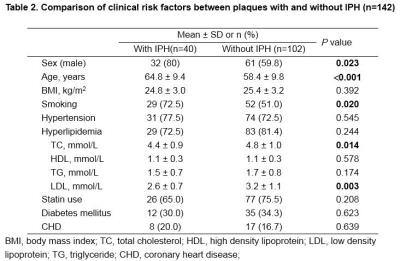
The clinical characteristics of this study population are summarized in Table 1. In this study population, 145 plaques were found in carotid arteries. Of these 145 plaques, 3 were excluded due to poor image quality (IQ=1). Of the remaining 142 carotid plaques, 40 (28.2%) had IPH and 92 (64.8%) had calcification. Table 2 presents the differences of clinical risk factors between plaques with and without IPH.
Correlation between carotid plaque calcification and IPH
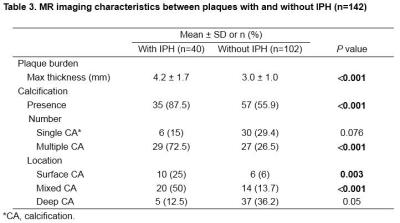
Compared with carotid plaques without IPH, those with IPH showed greater maximum wall thickness (4.2 ± 1.7mm vs. 3.0 ± 1.0mm, P<0.001) and prevalence of calcification (87.5% vs. 55.9%, P<0.001). In carotid plaques with IPH, the incidence of multiple calcification, surface calcification and mixed calcification was significantly higher than that of plaques without IPH (all P<0.05, Table 3). However, the difference of incidence of single calcification or deep calcification was not statistically significant between plaques with and without IPH (Table 3 and Figure 1).
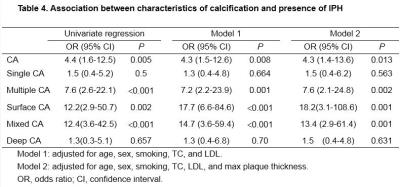
Table 4 showed the associations between characteristics of calcification and IPH in carotid plaques. In univariate regression analysis, presence of calcification (odds ratio [OR], 4.4; 95% confidence interval [CI], 1.6-12.5; P=0.005), multiple calcification (OR, 7.6; 95% CI, 2.6-22.1; P<0.001), surface calcification (OR, 12.2; 95% CI, 2.9-50.7; P<0.001), and mixed calcification (OR, 12.4; 95%CI, 3.6-42.5; P<0.001) were significantly associated with IPH. After adjusted for age, gender, smoke, TC and LDL (model 1) and age, gender, smoke, TC, LDL and maximum wall thickness (model 2), above associations remained statistically significant (all P<0.05, Table 4). In contrast, significant correlation was not found between presence of single calcification and deep calcification and IPH (both P>0.05, Table 4).
Discussion and conclusion
Surface calcification and multiple calcification in carotid atherosclerotic plaques are independently associated with presence intraplaque hemorrhage, suggesting that both quantity and location of calcification may play important role in plaque vulnerability. Biomechanics may shed light on the relationship between surface calcification and angiogenesis. Surface calcification and multiple calcification may increase the local stress and interface surface area which may lead to the rupture of neovessels and occurence of IPH. Our findings may provide the new insights into mechanism of intraplaque hemorrhage.Acknowledgements
This research was supported by the Fujian Science and Technology Project (Grant NO.2009Y0020), Natural Science Foundation of Fujian Province, China (Grant No.2015J01396), and National Natural Science Foundation of China (81271536, 81361120402).References
1. Takaya N, Yuan C, Chu B, Saam T, Polissar NL, Jarvik GP, Isaac C, McDonough J, Natiello C, Small R. Presence of intraplaque hemorrhage stimulates progression of carotid atherosclerotic plaques a high-resolution magnetic resonance imaging study. Circulation. 2005;111:2768-2775
2. Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, Wrenn SP, Narula J. Atherosclerotic plaque progression and vulnerability to rupture angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25:2054-2061
3. Sun J, Song Y, Chen H, Kerwin WS, Hippe DS, Dong L, Chen M, Zhou C, Hatsukami TS, Yuan C. Adventitial perfusion and intraplaque hemorrhage a dynamic contrast-enhanced mri study in the carotid artery. Stroke. 2013;44:1031-1036
4. Xu X, Ju H, Cai J, Cai Y, Wang X, Wang Q. High-resolution MR study of the relationship between superficial calcification and the stability of carotid atherosclerotic plaque. Int J Cardiovasc Imaging. 2010;26 Suppl 1:143-150
5. Van Den Bouwhuijsen QJ, Bos D, Ikram MA, Hofman A, Krestin GP, Franco OH, Van der Lugt A, Vernooij MW. Coexistence of calcification, intraplaque hemorrhage and lipid core within the asymptomatic atherosclerotic carotid plaque: The Rotterdam study. Cerebrovasc Dis. 2015;39:319-324
6. Eisenmenger L, Aldred B, Kim S-E, Stoddard G, de Havenon A, Treiman G, Parker D, McNally J. Prediction of carotid intraplaque hemorrhage using adventitial calcification and plaque thickness on CTA. AJNR Am J Neuroradiol. 2016;37:1496-1503
7. Zhou Z, Li R, Zhao X, He L, Wang X, Wang J, Balu N, Yuan C. Evaluation of 3d multi-contrast joint intra-and extracranial vessel wall cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance. 2015;17:41
8. Kerwin W, Xu D, Liu F, Saam T, Underhill H, Takaya N, Chu B, Hatsukami T, Yuan C. Magnetic resonance imaging of carotid atherosclerosis: Plaque analysis. Topics in Magnetic Resonance Imaging. 2007;18:371-378
Figures