0337
Noninvasive Functional Evaluation of Coronary Stenosis Using MR Instantaneous wave-Free Ratio (MR-iFR): Pilot patient study using invasive fractional flow reserve as a reference1Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Bioengineering, University of California, Los Angeles, Los Angeles, CA, United States, 3Cardiology, Severance Cardiovascular Hospital, 4Siemens Healthcare R&D, 5Radiology, Severance Cardiovascular Hospital
Synopsis
In patients with suspected coronary artery disease undergoing invasive coronary angiography, approximately half has nonsignificant stenosis (stenotic lesions that may not induce ischemia), leading to frequent and unnecessary invasive procedures. Previously, we proposed a noninvasive technique for functional evaluation of coronary stenosis using PC-MRI and navier-stokes equations. In this study, we evaluated the feasibility of the technique in patients, using invasive fractional flow reserve as a reference. Good correlation was observed between noninvasive and invasive techniques with high specificity and negative-predictive-value, demonstrating the potential of the proposed technique in identifying patients with functionally nonsignificant stenosis and eliminating unnecessary invasive procedures.
Purpose
In patients with suspected coronary artery disease (CAD) undergoing invasive coronary angiography (ICA), approximately half results in nonsignificant stenoses (<50% diameter stenosis or fractional flow reserve, FFR>0.80), leading to frequent, unnecessary, invasive procedures1,2. FFR (ratio of pressure distal to proximal of a coronary stenosis) has shown promise in identifying functionally significant stenoses that may cause myocardial ischemia (FFR≤0.80), however, the technique is invasive3. Recent noninvasive technique, FFRCT (coronary computed tomography angiography, CCTA, with computational fluid dynamic simulations), has shown to decrease the number of unnecessary invasive procedures4, however, CCTA requires ionizing radiation and is more prone to artifacts caused by calcification5. In this study, we use phase-contrast (PC)-MRI and Navier-Stokes (NS) equations to derive pressure difference (ΔP) across a coronary stenosis, which is then used to estimate the instantaneous wave-free ratio (iFR)6, wherein measurements were obtained during diastole without adenosine, denoted as MR-iFR. We have previously shown the reproducibility of this technique in phantoms and healthy subjects7. This work aimed to evaluate the feasibility of the technique in patients using both invasive FFR and offline-derived invasive iFR6 as references.Methods
Patient characteristics: 28 patients with known or suspected CAD, scheduled for ICA were recruited. All patients had ≥1 coronary lesion (proximal and/or middle stenosis, 30-70%) detected by CCTA and/or ICA. Both aortic pressure (Pa) and pressure distal of the stenosis (Pd) during rest and stress were obtained during invasive catheterization. FFR and iFR indices were obtained from the console (Volcano) and calculated offline6, respectively.
ΔP estimation: Consecutive cross-sectional PC-MRI images and invasive pressure values were obtained at the same vessel segment of interest to ensure measurements were location matched. Specifically, three-directional velocities (Vz, Vx, Vy) were first acquired using 2D-PC-MRI and used for NS analysis and integration along a path to obtain ΔP7. Imaging parameters: in-plane spatial resolution = 0.5-0.6x0.5-0.6mm2, slice thickness = 3.2mm, consecutive imaging slices = 4-9, cardiac phase = 2(~70ms/phase), Venc = 30-50cm/s in all three directions, and imaging time = ~4min/slice at 3T (Trio, Siemens Healthcare, Germany). Two methods were explored to obtain ΔP. Velocities obtained from all three directions (ΔPMR) were first explored. As in-plane velocities are small and may have minimal contribution to the overall pressure drop, velocities from through-plane direction only (ΔPMR-vz) was also analyzed. Note that velocities used for ΔPMR-Vz calculations were not acquired separately in this study. Since the proposed technique measures the relative pressure (ΔP), invasive aortic pressure (Pa) values were used as a proof of concept to calculate the MR-iFR index: MR-iFR = Pd / Pa = (Pa - ΔP) / Pa.
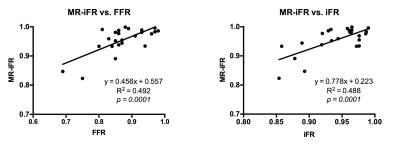
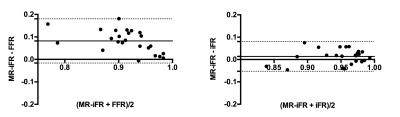
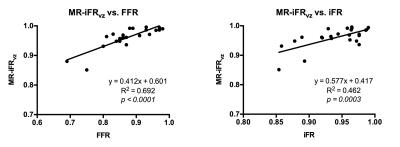
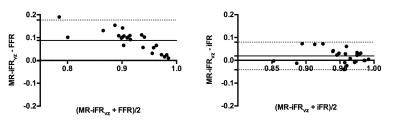
Data Analysis: Correlation of both MR-iFR and MR-iFRVz versus both FFR and iFR were assessed via linear regression analysis and agreement was assessed via Bland-Altman analysis.
Results
Good quality PC-MRI data were acquired in 24 (86%) patients where poor quality data were due to cardiac/respiratory motion. Three (12.5%) of the 24 patients had a functionally significant stenosis (FFR≤0.80). FFR, iFR, MR-iFR, and MR-iFRVz were 0.873±0.07, 0.941±0.04, 0.955±0.05, and 0.960±0.04, respectively. Good correlation r = 0.701/0.698 (p<0.001/0.001) (fig 1) and relatively small bias 0.082±0.05/0.014±0.03 (fig 2), were observed between FFR/iFR and MR-iFR, respectively. Similar results, r = 0.832/0.680 (p<0.001/0.001) (fig 3) and bias of 0.087±0.05/0.019±0.03 (fig 4), were observed between FFR/iFR and MR-iFRVz. Using FFR as gold standard and MR-iFR/MR-iFRVz cut off of 0.89, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were 67%/100%, 95%/95%, 67%/67%, and 95%/100%, respectively.Discussion
Slight difference was observed between MR-iFR and MR-iFRVz, however, not significant (p=0.22). Good correlation was observed for both MR-iFR and MR-iFRVz when comparing with invasive FFR and iFR. From Bland-Altman analysis, smaller bias was observed when comparing MR-iFR and MR-iFRVz with iFR, which is expected as the proposed method mimics more of an iFR technique. Interestingly, the highest correlation was between MR-iFRVz and FFR, suggesting the potential of using through-plane velocity direction only for estimating FFR. High specificity and NPV were observed for both MR-iFR and MR-iFRVz, demonstrating their potential in identifying patients with functionally nonsignificant stenoses and eliminating unnecessary invasive procedures. More patient studies with positive invasive FFRs are needed to further investigate the sensitivity of the approach and the utility of the MR-iFRVz method. Further technical improvements in terms of spatial, temporal resolutions and reduction of noise are being studied to further improve the accuracy of the proposed technique.Conclusion
Our pilot patient study demonstrated the feasibility of using PC-MRI to measure pressure gradient across coronary lesions. This approach has the potential to serve as a gatekeeper for unnecessary invasive catheterization procedures in patients with CAD.Acknowledgements
No acknowledgement found.References
1. Patel MR et al. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J. 2014 Jun; 167(6):846-52.
2. Tonino A.L. Pim et al. Angiographic Versus Functional Severity of Coronary Artery Stenoses in the FAME Study, J Am Coll Cardiol, 2010:55(25):2816-2821.
3. Tonino A.L. Pim et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 2009;360:213–224.
4. Nørgaard BL et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 2014;63:1145–1155.
5. Park MJ et al. Coronary CT angiography in patients with high calcium score: evaluation of plaque characteristics and diagnostic accuracy. Int J Cardiovasc Imaging 2011;27:43–51.
6. Sen S et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J. Am. Coll. Cardiol. 2012;59:1392–1402.
7. Deng et al. Pressure Gradient Measurement in the Coronary Artery Using Phase Contrast (PC)-MRI: Initial patient results towards noninvasive quantification of fractional flow reserve. ISMRM 2016, Velocity & Flow Quantification scientific session, #0319.
Figures