0335
Non-Gadolinium-Contrast Relaxation-Enhanced MR Angiography in Children with an Inversion Recovery and T2-Prepared 3D mDIXON Gradient-Echo Technique: Preliminary Experience1Radiology, Phoenix Children's Hospital, Phoenix, AZ, United States, 2Philips HealthTech, Dallas, TX, United States, 3Philips Electronics, Tokyo, Japan
Synopsis
We demonstrate the preliminary clinical feasibility and utility of a 3D non-Gadolinium MR angiography sequence called REACT (Relaxation-Enhanced MR Angiography without Contrast and Triggering) in 21 pediatric patients (age range: 1.7 – 16.1 years). REACT, which collectively utilizes T2-preparation, inversion recovery, and water-fat separation to suppress unwanted signals and exploit the long T1 and T2 times of unenhanced blood, is particularly beneficial in children, a population where Gadolinium administration should be minimized given recent concerns with residual intracranial Gadolinium deposition. We illustrate and compare REACT to Gadolinium-based MRA in the neck, upper and lower extremities, and the chest, abdomen, and pelvis.
Purpose
There has been growing evidence suggesting residual intracranial Gadolinium (Gd) deposition in pediatric and adult patients who undergo multiple contrast-enhanced MRI/A exams [1]. While Gd-based MRA scans remain common, emerging non-Gd MRA technique are attractive alternatives. In this work, we evaluate the feasibility and clinical utility of a new flow-independent non-Gadolinium 3D MRA technique in children. The sequence, called REACT (or Relaxation-Enhanced MR Angiography without Contrast and Triggering) facilitates visualization of the vasculature without the need for contrast agents. We highlight REACT in various anatomies and compare several results to corresponding Gd-enhanced MRA data.Methods
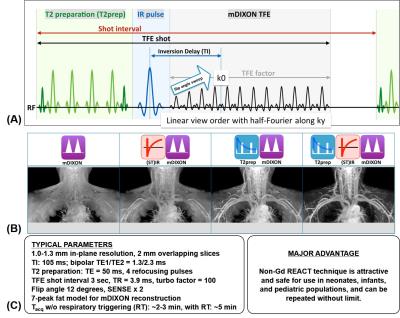
REACT: The REACT technique was previously described by Yoneyama, et al [2]. As shown in Figure 1a, the method is based on a conventional two-point 3D chemical-shift water-fat separated (mDIXON) TFE pulse sequence, with additional magnetization preparation by a non-volume-selective adiabatic inversion pulse preceded by a four-refocusing-adiabatic-pulse T2-prep module. As illustrated in Figure 1b, both the inversion recovery and the T2-prep modules are needed to collectively suppress signals from static tissues, such as muscles and organs with short T1 and T2 values, and to enhance the long T1 and T2 native signal of unenhanced blood for optimal vessel-to-background signal contrast. Typical imaging parameters used in this work are summarized in Figure 1c.
Experiments: With institutional review board approval and informed consent, we have to date successfully tested REACT across multiple anatomies in 21 patients with a variety of vascular pathologies, including two patients who had renal insufficiencies and therefore could not receive Gd administration. All imaging was implemented on a 3 Tesla platform (Philips Ingenia, software R5.1.7) using a 32-channel head coil, a 16-channel anterior torso coil array, and/or a 16-channel posterior spine coil built into the MRI table. In 19 cases, routine Gd-enhanced MRA acquired with mDIXON 3D spoiled gradient echo [3] and 2D post-Gd turbo-spin-echo sequences were also obtained. In these cases, REACT was performed prior to Gd-enhanced MRA scans.
Preliminary Analysis: Six pediatric body radiologists in consensus assessed qualitatively results from REACT to evaluate whether it was diagnostically useful either as a complement or potential replacement of Gd-MRA.
Results
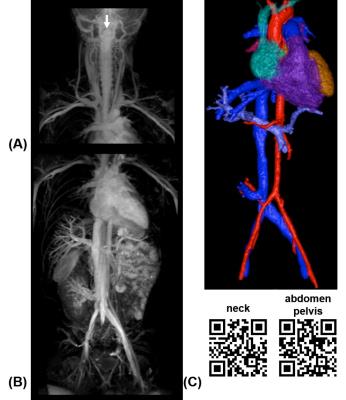
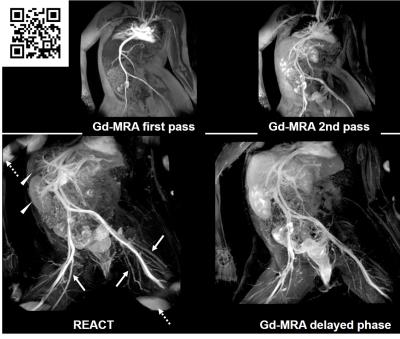
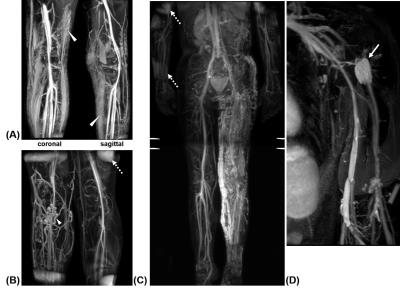
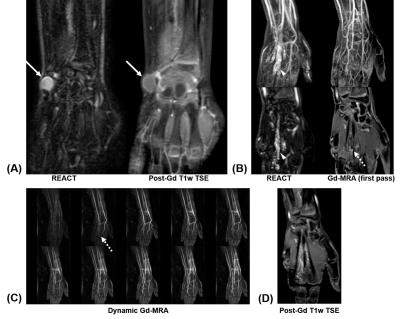
Several representative cases from our preliminary experience in children are shown in Figures 2-5. Figure 2 illustrates a case of the neck, chest, abdomen, and pelvis, in a patient with renal impairment and a history of multiple venous stenosis. The respiratory-triggered REACT results were able to clearly visualize patent bilateral internal jugular veins, subclavian and brachiocephalic veins, patent superior and inferior vena cava with no obvious filling defects, and a patent bilateral common iliac veins. Note in particular the well-visualized hepatic and renal vasculature on the patient’s right. Figure 3 illustrates a 12-years-old female who was referred for MRA with concerns of thrombosis of blood vessels in the chest, abdomen, and pelvis. Both REACT and Gd-MRA identified no areas of stenosis, dissection, or aneurysm. Note in particular from the figure the similar appearance of REACT to a delayed-phase Gd-MRA result. Figure 4 illustrates four examples of REACT in the upper and lower extremities. Note clear visualization of extensive edema (long T2 signals) in the subcutaneous adipose tissue anteriorly, cranially, and caudally in addition to the vasculature in Figure 4a. Figure 5 illustrates two additional examples in the wrist, highlighting the superior background tissue signal suppression of REACT as well as its clinical utility in assessing slow-flow vascular malformations as a supplement to Gd-MRA.
In the two patient cases where Gd-administration was not possible due to renal impairment, the radiologists agreed that REACT provided valuable vascular information that would otherwise have not been possible to obtain with MRI. In the remaining cases, REACT was found to be useful in 9 cases in potentially supplanting Gd-MRA without impacting clinical diagnosis, primarily in the chest, abdomen, and pelvis. Overall, the radiologists felt in this pilot study that the REACT sequence was complementary to Gd-MRA.
Discussion and Conclusion
Our preliminary experience with REACT in children suggests that the sequence is robust and capable of providing diagnostically useful angiograms across the body. The sequence appears promising and will facilitate additional MRA exams at our pediatric institution to be performed without Gd. REACT will be particularly useful in very young patients and in children who are renally impaired. One clear advantage of REACT is that it can be repeated without limits and is not constrained by asymmetric flow, thus obviating the need for concerns with sequence timings that are associated with Gd-MRA. Future work will evaluate whether REACT alone can provide a clinical diagnosis in specific pathologies such that Gd can be potentially avoided.
Acknowledgements
Phoenix Children's Hospital acknowledges research and funding support from Philips.References
[1] http://www.ismrm.org/mr-safety-links/gadolinium-retention-updates-and-resources/
[2] Yoneyama M, et al. Non-contrast, flow-independent, relaxation-enhanced subclavian MR angiography using inversion recovery and T2 prepared 3D gradient-echo DIXON sequence. Proceedings of the ISMRM, Singapore 2016; 24: abstract #2252.
[3] Leiner T, et al. Subtractionless first-pass single contrast medium dose peripheral MR angiography using two-point Dixon fat suppression. European Radiology 2013; 23(8): 2228-2235.
Figures