0332
Utilizing Quantitative Measurements of Carotid Intraplaque Hemorrhage can Improve on Presence Alone in Classifying Patients with and without Acute Cerebral Infarcts1Department of Radiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, People's Republic of China, 2Department of Vascular disease, Beijing Anzhen Hospital, Capital Medical University, Beijing, People's Republic of China, 3Department of Radiology, University of Washington, Seattle, WA, United States
Synopsis
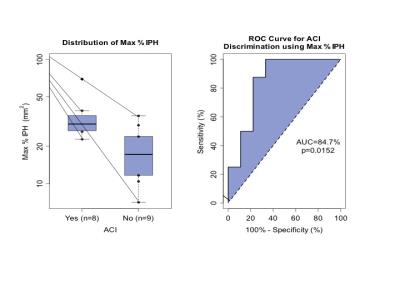
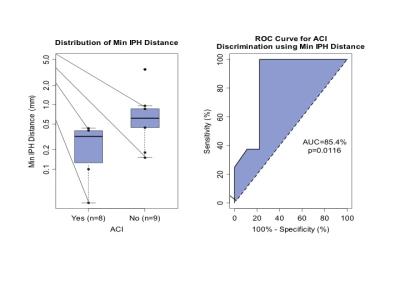
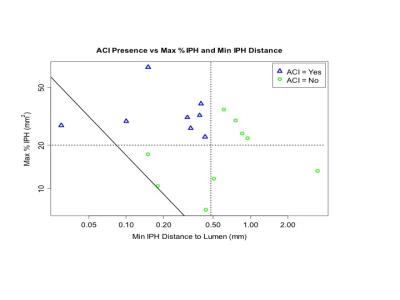
Histological studies have shown that intraplaque hemorrhage (IPH) size might be important in assessing disease severity. We hypotheses that the quantitative measurements of IPH by MRI provide additional value towards classify acute cerebral infarcts (ACI) in the carotid territory by brain MRI. We found that the subjects with ACI had larger max % IPH measurements (AUC=84.7%, p=0.015) and IPH closer to the lumen (AUC=85.4%, p=0.012). Further, using the size and distance measurements simultaneously improved the AUC to 96.9%. Beyond the presence of IPH, quantitative measurements of IPH may improve the predictive value of carotid plaque imaging for future stroke.
Background
Intraplaque hemorrhage (IPH) in the carotid atherosclerotic lesion has been identified as a key component that significantly triggers disease progression. From in vivo natural history studies with carotid MRI, the presence of IPH has been associated with accelerated expansion of plaque burden and increased luminal narrowing1,2. Histological studies have shown that intraplaque hemorrhage (IPH) size might be important in assessing disease severity3.Purpose
This study was to investigate whether the quantitative measurements of IPH (e.g. size and its distance to the lumen) can provide additional value towards predicting acute cerebral infarcts (ACI) in the carotid territory.Method
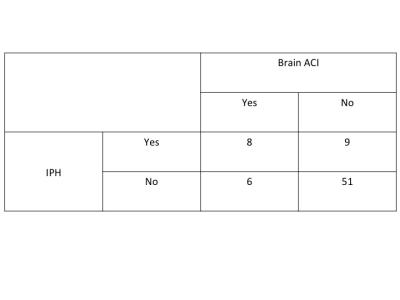
A total of 77 patients with >or=50% carotid stenosis by duplex ultrasound underwent multi-contrast carotid and brain MRI scans at 3T. Carotid MRI scans were performed using a high-resolution multi-contrast protocol, including TOF, T2W, IW, and pre- and post-contrast T1W imaging. MR imaging of the brain was subsequently performed including T1W, T2W, and diffusion weighted imaging (DWI). Two radiologists reviewed carotid images and brain images independently. From carotid MRI, two quantitative measurements for IPH—max % size (maximum value of IPH area / wall area x 100% over all slices) and minimum distance to the lumen—were measured using a custom-designed image analysis tool. From brain MRI, the presence of ACI in the ipsilateral carotid territory was recorded according to DWI images. Diagnostic accuracy was assessed using sensitivity and specificity for binary variables and area under the ROC curve (AUC) for continuous variables. Logistic regression was used to combine continuous variables into a single predictor.Results
Two subjects were excluded due to poor image quality and one was excluded due to total occlusion. Of the remaining subjects (n=74), 17 (23%) had IPH and 14 (19%) had ACI. The presence of IPH was significantly associated with the presence of ACI (OR=7.6, p=0.002). Only the subjects with IPH (n = 17) were used to assess the quantitative IPH measurements. Of those, the subjects with ACI had larger max % IPH measurements (AUC=84.7%, p=0.015) and IPH closer to the lumen (AUC=85.4%, p=0.012). Further, using the size and distance measurements simultaneously improved the AUC to 96.9%.Discussion
The results demonstrate that compared with intraplaque hemorrhage presence alone, quantitative measurements of the size and proximity of intraplaque hemorrhage to the lumen contribute additional valuable information regarding likelihood of acute cerebral infarcts in subjects with advanced carotid atherosclerosis. For the clinical application, beyond the presence of intraplaque hemorrhage, quantitative measurements of intraplaque hemorrhage may improve the predictive value of carotid plaque imaging for future stroke.Acknowledgements
No acknowledgement found.References
1. Takaya N, Yuan C, Chu B, et al. Presence of intraplaque hemorrhage stimulates progression of carotid atherosclerotic plaques: a high-resolution magnetic resonance imaging study. Circulation 2005, 111(21):2768–75
2. Sun J, Underhill HR, Hippe DS, et al. Sustained acceleration in carotid atherosclerotic plaque progression with intraplaque hemorrhage: a long-term time course study. JACC Cardiovasc Imaging. 2012 Aug;5(8):798-804
3. Kolodgie FD, Gold HK, Burke AP, et al. Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med 2003, 349(24):2316–25
4. Saam T, Ferguson MS, Yarnykh VL, et al. Quantitative evaluation of carotid plaque composition by in vivo MRI. Arterioscler Thromb Vasc Biol 2005;25:234-9
5. Kerwin W, Xu D, Liu F, et al. Magnetic resonance imaging of carotid atherosclerosis: plaque analysis. Top Magn Reson Imaging 2007; 18: 371–378
Figures