0323
Insulinoma localization with cross-sectional imaging: head-to-head comparison of contrast-enhanced CT, volume perfusion CT and multi-parametric MR1Radiology, Peking Union Medical College Hospital, Beijing, People's Republic of China, 2MR collaborations NE Asia, Siemens Healthcare, Beijing, People's Republic of China
Synopsis
This study aims to compare insulinoma localization with CECT, VPCT and multi-parametric MR (mp-MR) at 3T in the same patients, in a prospective manner. CECT, VPCT and mp-MR were performed in patients with suspected insulinomas. The presence/absence of tumor within the pancreatic head, neck, body and tail region was evaluated with 5-scale confidence levels. ROC analysis was performed. Surgical pathology served as reference standard. We found that VPCT and mp-MR showed improved diagnostic performance for insulinoma localization, compared to CECT. Both modalities could serve as problem-solving tools in difficult cases. mp-MR has the potential to replace CECT as the first-line examination.
Introduction
Insulinomas are the most common hyper-functioning pancreatic endocrine tumors (PETs). Knowing the exact number and location of tumors is pivotal for surgery planning. Historically, detection of insulinomas by cross-sectional imaging has been difficult [1,2]. Nowadays, a greater sensitivity for insulinoma detection has been reported with state-of-the-art CT and MR scanners [3,4,5]. However, which modality and which protocol provides best diagnostic accuracy remains unknown. The purpose of this prospective study is to compare the diagnostic performance of biphasic contrast-enhanced CT (CECT), volume perfusion CT (VPCT) and multi-parametric MR (mp-MR) at 3T, in patients with clinically suspected insulinomas.
Methods
CT protocol Biphasic CECT and VPCT examinations were performed on a SOMATOM FLASH 128-detector CT scanner (Siemens Healthcare, Forchheim, Germany). After non-enhanced scan of the upper abdomen, biphasic scans including arterial phase and portal venous phase were obtained. After a 15-minute interval, the volume perfusion scan was performed, which consisted of 25 acquisitions of 0.5 s duration every 1.5 s. MR protocol mp-MR was performed on a MAGNETOM Skyra 3T MR scanner (Siemens Healthcare, Erlangen, Germany). An 18-channel phased array body coil (anterior) and 16 channels of the spine coil (posterior) were used in combination for signal reception. The mp-MR protocol consisted of breath-hold T1-weighted Dixon sequence, T2-weighted HASTE sequence, T2-eighted BLADE sequence with and without fat suppression, and free-breathing multi-b-value trace-weighted EPI DWI (b value=50,200,400,600,800 s/mm²). All T2-weighted sequences and DWI sequences were respiratory triggered. Image analysis Two readers independently evaluated the presence/absence of tumor within the pancreatic head, neck, body and tail region, using a 5-scale scoring system. CECT, VPCT and mp-MR were independently evaluated, irrespective of findings on other imaging work-ups. When a tumor was considered present (score 4-5) on imaging, tumor size was recorded. Surgical results served as reference standard. Receiver operating characteristic analysis was performed. Statistical analysis The receiver operating characteristic (ROC) curve was generated to compare the diagnostic performance of biphasic CT, VPCT, and MR. Inter-observer agreement for each image set was assessed.Results
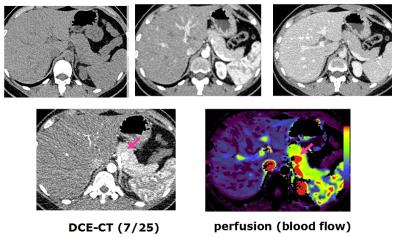
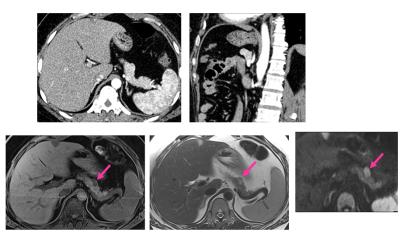
Eighteen tumors were surgically removed. The mean tumor size was 1.3±0.5cm. CECT revealed a lower area under the curve (AUC)(0.78) compared to VPCT (0.99,p<0.01) and mp-MR (0.97,p<0.01). A sum score combining CECT and MR yielded an AUC of 0.99, whereas a sum score combining CECT and VPCT yielded an AUC of 0.96. For tumors less than 1 cm in size (n=8), CECT+VPCT showed the highest AUC (0.92). Tumor size measured on DWI (b=800 s/mm²) was most accurate, followed by arterial-phase CT images. There was good to excellent agreement between observers (k=0.64 for CECT, 0.80 for VPCT, and 0.84 for mp-MR).Figure 1 shows a case, in which a 1.1-cm insulinoma in the pancreatic body was missed using biphasic CECT,but detected with high diagnostic confidence using VPCT. The tumor remains isoattenuating on arterial-phase and portal-venous-phase images. By observing the dynamic enhanced images with higher resolution from VPCT, the tumor was found to demonstrate a transient hyper-enhancement pattern and was best appreciated at the 7th of 25 dynamic phases. The pseudo-colored perfusion map also revealed the tumor as a nodule with high blood flow.Figure 2 shows a case, in which a tumor was suspected but with low diagnostic confidence on biphasic CT. It appeared as a slightly hyperenhancing nodule protruding from the pancreatic contour. mp-MR clearly demonstrates the tumor as a moderately hypointense nodule on T1-weighted fat suppressed images, a slightly hyperintense nodule on T2-weighted images, and a markedly hyperintense nodule on high-b-value DWI images. The diagnostic confidence was greatly improved with mp-MR.Discussion
In this intra-individual comparative study, VPCT and mp-MR had similar high accuracy in insulinoma detection, and both were significantly more accurate than biphasic CECT. The main reason that CECT fails to detect an insulinoma is that the tumor remains isoattenuating to pancreatic parenchyma [6]. VPCT has higher temporal resolution, and was able to reveal the transient hyperenhancement of the tumor missed by biphasic CT [7]. However, the drawback of VPCT is the higher radiation dose. High diagnostic accuracy was also achieved with mp-MR. The intrinsic superior soft-tissue contrast helps to identify the tumor more easily without using contrast agents. Since insulinomas are quite small, the improved signal-to-noise of 3T MR compared to 1.5T and the introduction of high-resolution DWI might explain the higher diagnostic performance compared to previous reports.Conclusion
VPCT and mp-MR showed improved diagnostic performance for insulinoma localization.Acknowledgements
NoneReferences
1. Norton JA, Shawker TH, Doppman JL, Miller DL, Fraker DL, et al. (1990) Localization and surgical treatment of occult insulinomas. Ann Surg 212: 615-620. 2. Doherty GM, Doppman JL, Shawker TH, Miller DL, Eastman RC, et al. (1991) Results of a prospective strategy to diagnose, localize, and resect insulinomas. Surgery 110: 989-996; discussion 996-987. 3. Thoeni RF, Mueller-Lisse UG, Chan R, Do NK, Shyn PB (2000) Detection of small, functional islet cell tumors in the pancreas: selection of MR imaging sequences for optimal sensitivity. Radiology 214: 483-490. 4. Ichikawa T, Peterson MS, Federle MP, Baron RL, Haradome H, et al. (2000) Islet cell tumor of the pancreas: biphasic CT versus MR imaging in tumor detection. Radiology 216: 163-171. 5. Brenner R, Metens T, Bali M, Demetter P, Matos C (2012) Pancreatic neuroendocrine tumor: added value of fusion of T2-weighted imaging and high b-value diffusion-weighted imaging for tumor detection. Eur J Radiol 81: e746-749. 6. Zhu L, Xue HD, Sun H, Wang X, He YL, et al. (2016) Isoattenuating insulinomas at biphasic contrast-enhanced CT: frequency, clinicopathologic features and perfusion characteristics. Eur Radiol 26, no. 10 (2016): 3697-705. 7. Zhu, L., Xue HD, Sun H, et al., Insulinoma detection with MDCT: is there a role for whole-pancreas perfusion?. AJR Am J Roentgenol, 2016 epub ahead of print, doi: 10.2214/AJR.16.16351Figures