0289
Multiparametric Assessment of Patients with Aortic Stenosis using Multipoint 4D Flow MRI - Correlation with Cardiac Biomarkers1Institute for Biomedical Engineering, University & ETH Zurich, Zurich, Switzerland, 2Department of Cardiology, University Hospital Zurich, Zurich, Switzerland
Synopsis
Various flow characteristics, such as Turbulent Kinetic Energy (TKE), flow displacement or jet angle, derived from 4D Flow MRI, have been used to investigate the hemodynamic effects of aortic stenosis (AS). However, the predictive value of these flow parameters is still unknown. Therefore, we investigated the correlation between multiple flow parameters and cardiac biomarkers which are known to provide prognostic information on the progression and outcome of AS. Our results revealed that MRI-based TKE and peak velocity significantly correlate with NT-proBNP, implying potential relevance of these imaging parameter for future risk stratification of AS patients.
Introduction
Aortic stenosis (AS) is the most prevalent valvular heart disease and is associated with a high mortality when symptoms occur [1]. The echocardiographic measures of Mean Pressure Gradient (MPG) and aortic valve area (AVA), which the diagnosis of AS is based on according to current guidelines [2], do not account for post-stenotic pressure recovery and are known to be poorly correlated with prognostic cardiac biomarkers [3]. In recent studies, various flow characteristics, such as Turbulent Kinetic Energy (TKE), flow displacement or jet angle derived from 4D Flow MRI have been used to investigate the hemodynamic effects of AS. It has been found that probing energy losses due to AS by the measurement of TKE, allows assessing the influence of valve morphology and aortic geometry on the hemodynamic burden of AS [4] and that normalized flow displacement is associated with LV remodeling [5]. However, longitudinal studies for the assessment of the prognostic value of these flow parameters are still missing. Therefore, we sought to investigate the correlation between multiple flow parameters and cardiac biomarkers including NT-proBNP, which are known to provide important prognostic information on the progression and outcome of AS patients.Methods
For this ongoing study, 41 patients with aortic stenosis (69±14 years, 17 female) were prospectively recruited. All subjects underwent time-resolved 3D Phase-Contrast MRI (4D Flow MRI) in addition to a routine cardiac MRI protocol and an echocardiography examination. Data were acquired on a clinical 3T system (Philips Healthcare, Best, The Netherlands) using a 4D Bayesian MultiPoint PC-MRI sequence [6] with 8-fold k-t PCA [7] acceleration and three velocity encoding steps in each direction. Prospective cardiac triggering and respiratory navigation allowed for acquisition during free-breathing with an isotropic spatial resolution of 2.5x2.5x2.5mm3. TKE was computed voxelwise and integrated over the ascending aorta and the aortic arch. For analysis, peak systolic values (TKEpeak) and the systolic TKE, normalized for stroke volume (normTKEsys) are reported. In addition, the peak velocity, the angle of the flow jet in relation to the direction of the vessel and the normalized flow displacement were assessed. In all patients, NT-proBNP was measured, corrected for renal function [8] and indexed for the age- and gender-specific reference value. In 33 patients, hs-Troponin T was additionally available.Results
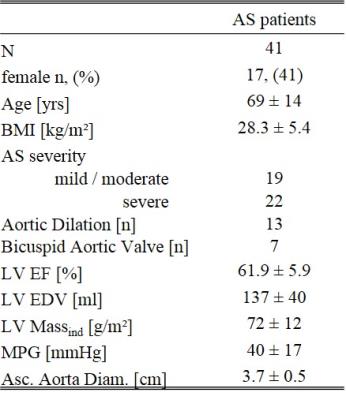
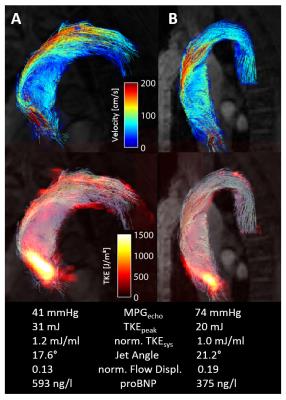
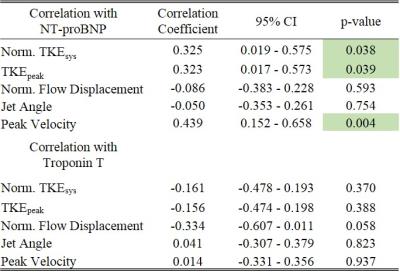
According to the echocardiographic assessment, 22 patients had severe AS (MPG ≥ 40 mmHg) and 19 had mild/moderate AS (see table 1 for baseline characteristics). Elevated NT-proBNP levels were present in 18 patients and 11 patients had pathologically high hs-Troponin T values. Indexed NT-proBNP was significantly correlated with TKEpeak (r=0.323, p<0.05), normTKEsys (r=0.325, p<0.05) and peak velocity (r=0.439, p<0.01), while no significant correlation with the jet angle or flow displacement could be found. Hs-TroponinT was not correlated with any flow parameter derived from 4D Flow MRI (see Table 2 for the detailed results). Figure 1 illustrates flow fields and TKE distributions with the corresponding flow parameters of two patients with severe AS. Compared with Pat A, Pat B has a higher echocardiographic MPG while both TKE and NT-proBNP are lower.Discussion
NT-proBNP is a cardiac biomarker that independently predicts symptom-free survival in patients with AS [9]. Its correlation with TKE and peak velocity implies that these parameter may also exhibit prognostic information for this patient cohort. Peak velocity, however, is directly related to the echocardiographic pressure gradient via the Bernoulli equation and thereby does not justify the use of an advanced imaging technique like MR for its determination. In contrast, TKE is only assessable by 4D Flow MRI. To this end our results warrant future longitudinal studies to unambiguously identify a potential prognostic information of the energy loss due to turbulent flow and its value for risk stratification in AS patients. Isolated flow characteristics such as the jet angle and flow displacement did not correlate with NT-proBNP. In addition, hs-Troponin T as a marker for acute myocardial damage did not correlated with any imaging parameter. This finding may be because the pressure overload that AS poses on the heart causes long term myocardial remodeling instead of acute cell death.
In summary, the correlation of TKE and peak velocity derived from 4D
Flow MRI with NT-proBNP implies that those parameters may provide prognostic information on the
hemodynamic burden of AS.
Acknowledgements
No acknowledgement found.References
1. Iung et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231–1243.
2. Vahanian et al. Guidelines on the management of valvular heart disease (version 2012): The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2012;33:2451–2496
3. Ben-Dor et al. Correlation of brain natriuretic peptide levels in patients with severe aortic stenosis undergoing operative valve replacement or percutaneous transcatheter intervention with clinical, echocardiographic, and hemodynamic factors and prognosis. Am J Cardiol. 2013;112:574-579
4. Gotschy et al. Added Value of Phase-Contrast MRI based Turbulent Kinetic Energy Quantification for the Assessment of Aortic Stenosis Severity. Proc. Intl. Soc. Mag. Reson. Med. 24 (2016) 0464
5. von Knobelsdorff-Brenkenhoff et al. Evaluation of Aortic Blood Flow and Wall Shear Stress in Aortic Stenosis and Its Association With Left Ventricular Remodeling. Circ Cardiovasc Imaging. 2016;9:e004038.
6. Binter et al. Bayesian multipoint velocity encoding for concurrent flow and turbulence mapping. Magn Reson Med. 2012/06/16 ed. 2013;69:1337–1345
7. Pedersen et al. k-t PCA: Temporally Constrained k-t BLAST Reconstruction Using Principal Component Analysis. Magn Reson Med. 2009;62:706–716
8. Luchner et al. Improvement of the cardiac marker n-terminal-pro brain natriuretic peptide through adjustment for renal function: A stratified multicenter trial. Clin Chem Lab Med. 2010;48:121-128
9. Bergler-Klein et al. Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation. 2004;109:2302-8.
Figures