0287
Multi-year 4D flow MRI Follow-Up Study of Bicuspid and Tricuspid Aortic Valve patients and Association between Wall Shear Stress and Aortic Diametric GrowthOzair Rahman1, Alex Barker2, Carmen Blanken2, Emilie Bollache2, Michael Rose3, Pim Van Ooji2, Jeremy Collins2, James Carr2, Chris Malaisrie4, Patrick McCarthy4, and Michael Markl2
1Radiology, Northwestern University, Chicago, IL, United States, 2Radiology, Northwestern University, 3Radiology, Ann & Robert H. Lurie Children's Hospital of Chicago, 4Cardiac Surgery, Northwestern University
Synopsis
Patients with Bicuspid Aortic Valve (BAV) are at increased risk of developing aortopathy compared to Tricuspid Aortic Valve (TAV) patients. However, there is imited data presenting the development of pathophysiologic changes taking place over multi year time period. Our study attempts to quantify the changes that take place from baseline and follow-up scans to help us better understand this process.
Introduction
Patients with bicuspid aortic valve (BAV) are known to be at higher risk for the development of aortopathy (aortic dilatation, aneurysm, and dissection) compared to patients with normal trileaflet valves (TAV)1. Previous 4D flow MRI studies have shown that valve mediated changes in aortic hemodynamics, such as elevated peak velocity (PV) or altered wall shear stress (WSS), are associated with aortic dilatation2, 3. However, there is limited data on the potential value of these parameters to predict which patients are at risk for development of aortopathy. In this multiyear follow-up 4D flow MRI study, we assessed long-term changes in the ascending aortic WSS and PV and their association with progressive aortic dilatation in both BAV and TAV patients.Methods
A retrospective IRB approved and HIPAA compliant study was conducted in patients with bicuspid (BAV, n=45, age: 44±12 years) or tricuspid (TAV, n=17, age: 69±5 years) aortic valve and aneurysmal dilatation (>4.0 cm) of the ascending aorta (AAo), and healthy TAV ‘controls’ (n=9, age: 50±15 years), who underwent baseline and follow-up aortic 4D flow MRI exams (follow-up duration: 2.66±0.66 years for BAV; 2.56±0.43 years for TAV; 1.09±0.48 years for controls). 4D flow MRI data analysis included noise filtering, correction of Maxwell terms and Eddy currents as well as velocity aliasing, 3D segmentation of the thoracic aorta and subsequent quantification of systolic PV and 3D WSS maps in the AAo (Figure 1). Systolic WSS was quantified as the average over the entire AAo wall surface. In addition, aortic diameters at the sinus of Valsalva (SOV) and mid AAo (MAA) as well as AAo volume were determined at baseline and follow-up using contrast-enhanced MR angiograms.Results
SOV and MAA diametric growth from baseline to follow-up was observed in patients with BAV (SOV: 3.9 ± 0.34 to 4.08 ± 0.36 cm; P=0.0003, MAA: 4.02 ± 0.51 to 4.13 ± 0.55 cm; P=0.0005) and also TAV (SOV: 4.3 ± 0.20 to 4.32 ± 0.35 cm; P=0.04, MAA: 3.56 ± 0.50 to 3.69 ± 0.48 cm; P=0.001) patients (Table 1). This increase in aortic dilation was accompanied by a significant increase in PV (P=0.0006) in BAV but no significant change was seen in patients with TAV (P=0.69) (Figure 2). Patients with BAV also had a notable decrease in WSS in the AAo (0.74 ± 0.21 to 0.65 ± 0.22 Pa; P<0.0001) but not in TAV patients (0.45 ± 0.12 to 0.47 ± 0.16 Pa; P=0.64), whose WSS measurements remained steady from baseline to follow-up.Discussion
Progressive aortic dilatation was seen in patients with BAV and TAV with aortic dilation over an average of 2.66 years follow-up (rate of 0.5-1mm per year). These findings correspond to the literature4. Interestingly, the WSS changes were only noted in BAV and not seen in either TAV cohorts. This decrease in WSS together with an increase in peak velocity might point to a specific pathophysiologic mechanism involved in the development of aortic dilation in patients with BAV.Conclusion
The findings of this study show that WSS changes are seen in patients specifically with BAV, and not in patients with TAV. This follow-up study lends credence to the compensation on a cellular level-taking place in the aorta. Future investigations should include patients with longer follow-up times and multiple scans for each patient to better understand the development of aortopathy over time in patients with BAV.Acknowledgements
No acknowledgement found.References
[1] Michelena HI, Della Corte A, Prakash SK, Milewicz DM, Evangelista A, Enriquez-Sarano M. Bicuspid aortic valve aortopathy in adults: Incidence, etiology, and clinical significance. Int J Cardiol 2015;201:400-7. [2] Saikrishnan N, Mirabella L, Yoganathan AP. Bicuspid aortic valves are associated with increased wall and turbulence shear stress levels compared to trileaflet aortic valves. Biomech Model Mechanobiol 2015;14(3):577-88. [3] Mahadevia R, Barker AJ, Schnell S, et al. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation 2014;129(6):673-82. [4] Ruzmetov M, Shah JJ, Fortuna RS, Welke KF. The Association Between Aortic Valve Leaflet Morphology and Patterns of Aortic Dilation in Patients With Bicuspid Aortic Valves. Ann Thorac Surg 2015;99(6):2101-7; discussion 7-8.Figures

Figure 2: Evolution
from baseline (blue bars) to follow-up (orange bars) of WSS (A), Peak Velocity
(B), and Diametric changes in both the Sinus of Valsalva (C) and Mid Ascending
Aorta (D) in patients with BAV, TAV with aneurysmal growth, and “Controls”.
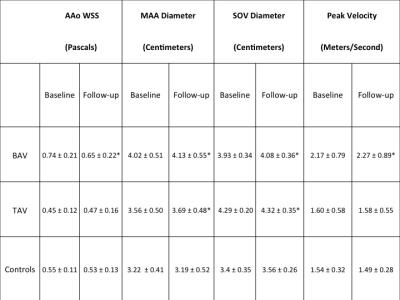
Table 1: Ascending
aortic WSS, MAA and SOV Diameter as well as Peak Velocity at baseline and
follow-up in BAV patients and TAV patients with and without dilatation of the
AAo at baseline. *statistically significant when compared to baseline
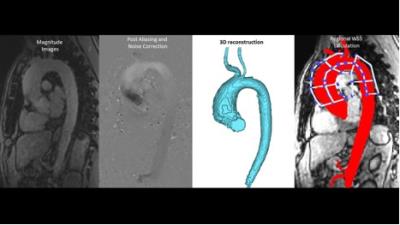
Figure 1: Stepwise
process of aortic 4D flow image processing (Noise reduction, anti-aliasing, and
eddy current correction), 3D volume segmentation and regional WSS
quantification with delineation of the Ascending Aorta from the root to the
innominate branch.