0275
Determinants of Symptomatic Intracranial Atherosclerotic Plaque Enhancement on 3D DANTE T1-SPACE Vessel Wall MRI and Relationship to Recurrent Stroke or TIA1Neurology, University of Utah, Salt Lake City, UT, United States, 2Radiology, University of Utah, Salt Lake City, UT, United States, 3Neurology, University of Washington, Seattle, WA, United States
Synopsis
Intracranial atherosclerotic enhancement on vessel wall MRI is associated with with symptomatic plaque, but there is insufficient data on the clinical characteristics associated with atherosclerotic enhancement on T1-weighted vessel wall MRI sequences or the relationship between atherosclerotic enhancement and recurrent stroke or TIA. Our study demonstrates that intracranial atherosclerotic plaque enhancement detected on 3T vessel wall MRI with 3D DANTE T1-SPACE accurately predicts a high risk of early stroke or TIA recurrence, with a potentially modifiable risk factor: elevated serum hemoglobin A1c.
Purpose:
Prior studies have linked atherosclerotic enhancement with symptomatic intracranial plaque,1,2 but there is insufficient data on the clinical characteristics associated with atherosclerotic enhancement on T1-weighted vessel wall MRI sequences or the relationship between atherosclerotic enhancement and recurrent stroke or TIA.
Methods:
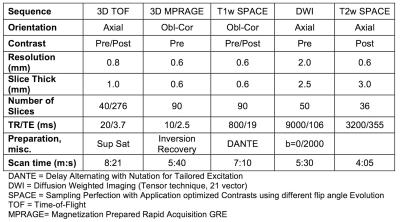
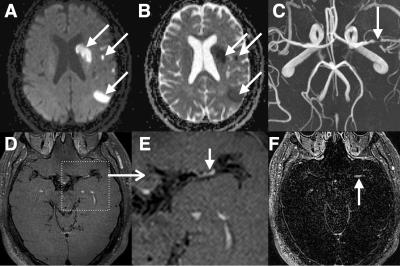
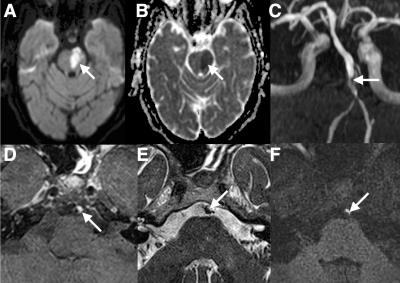
We included patients with acute ischemic stroke or TIA, <8 days from onset, due to intracranial atherosclerosis. Key exclusion criteria included atrial fibrillation or alternate stroke etiologies such as vasculitis or carotid stenosis. All intracranial vessel wall MRIs were performed on a 3T Siemens Verio or Trio with a 20-channel head coil. Vessel wall MRI was interpreted by 4 experienced neuroradiologists and confirmed by a vascular neurologist, using a multicontrast approach of 3D TOF, T1- and T2-weighted sequences3 (Table 1). Atherosclerotic plaque enhancement was measured in the stroke parent artery on postcontrast T1-weighted SPACE with DANTE preparation for blood signal suppression4 (Figures 1 and 2). Plaque enhancement was considered ‘mild’ if visually apparent but less intense than the cavernous sinus and ‘intense’ if greater or equal in intensity to the cavernous sinus. The outcome of recurrent stroke or TIA in the index stroke parent artery distribution was ajudicated by a vascular neurologist who was blinded to the vessel wall MRI results. Statistical comparisons were performed with Student’s t-test, Fisher’s exact test, Chi-2 test, and Cox proportional hazards models, where patients were censured at the time of last clinical follow-up or recurrent stroke or TIA.Results:
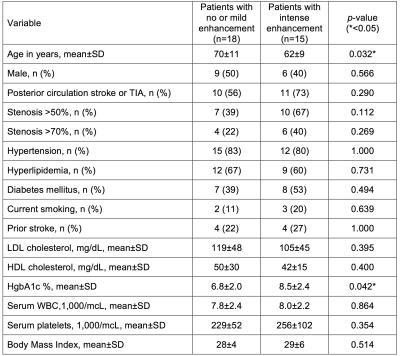
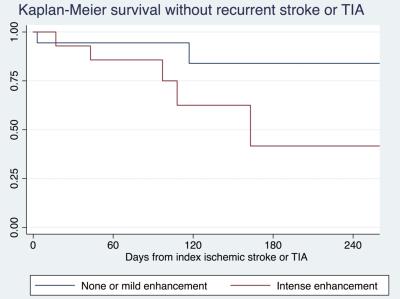
33 patients met inclusion criteria, of which 29/33 (88%) had stroke as the index event. Time from index event to MRI was 2.5±1.6 days. Atherosclerotic enhancement of the stroke parent artery was present in 25/33 (76%), of which 15/33 (46%) were intense and 10/33 (30%) were mild. Stroke parent artery stenosis was >50% in 17/33 (52%) and >70% in 10/33 (30%). Clinical determinants of intense atherosclerotic enhancement are seen in Table 2, of which younger patient age and higher hemoglobin A1c were significantly associated with intense atherosclerotic enhancement. Recurrent stroke or TIA occurred in 9/33 (27%) of patients (5/9 with stroke) at 120±98 days, and in the remainder of patients the mean days of follow-up without stroke or TIA was 104±75 days. All 9 patients with recurrence had atherosclerotic enhancement (p=0.047), of which 6/9 were intense and 3/9 were mild. In the Cox model, after controlling for patient age, intense atherosclerotic enhancement had a hazard ratio of 4.5 for recurrent stroke or TIA (p=0.018) (Figure 3). Neither stenosis cutoffs, >50% nor >70%, were predictive of recurrent stroke in the Cox model (p=0.188, 0.112), likely due to the limited follow-up period.Discussion:
In patients with recently symptomatic intracranial atherosclerosis, intense plaque enhancement was an accurate predictor of early stroke or TIA recurrence, with a hazard ratio of 4.5. Determinants of intense plaque enhancement included younger patient age and higher HgbA1c, the later of which has implications for secondary prevention research. In the SAMMPRIS trial, the yearly rate of stroke recurrence was 12.2% in the medical management group.5 Our study differed from that pivotal trial because we included all levels of stenosis. Nonetheless, the extrapolated yearly recurrent stroke rate for patients with intense atheroslceortic enhancement would be ~30%, which is consistent with recently pubished data from an Asian cohort.6 This supports the concept that atherosclerotic enhancement is a more accurate predictor of stroke risk than stenosis alone, particularly in the sub-acute period.Conclusion:
Intracranial atherosclerotic plaque enhancement detected on 3T vessel wall MRI with 3D DANTE T1-SPACE accurately predicts a high risk of early stroke or TIA recurrence, with a potentially modifiable risk factor: elevated serum hemoglobin A1c.Acknowledgements
NoneReferences
1. de Havenon, A, Chung L, Park, M, Mossa-Basha, M. Intracranial vessel wall MRI: a review of current indications and future applications. Neurovascular Imaging 2016;2(10).
2. Dieleman N, Kolk AG van der, Zwanenburg JJM, et al. Imaging Intracranial Vessel Wall Pathology With Magnetic Resonance Imaging Current Prospects and Future Directions. Circulation 2014;130(2):192–201.
3. Mossa-Basha M, Hwang WD, De Havenon A, et al. Multicontrast high-resolution vessel wall magnetic resonance imaging and its value in differentiating intracranial vasculopathic processes. Stroke J Cereb Circ 2015;46(6):1567–73.
4. Li L, Chai JT, Biasiolli L, et al. Black-blood multicontrast imaging of carotid arteries with DANTE-prepared 2D and 3D MR imaging. Radiology 2014;273(2):560–9.
5. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 2011;365(11):993–1003.
6. Kim J-M, Jung K-H, Sohn C-H, et al. Intracranial plaque enhancement from high resolution vessel wall magnetic resonance imaging predicts stroke recurrence. Int J Stroke 2016;11(2):171–9.
Figures