0268
ASPECTS Based Reperfusion Status on Arterial Spin Labeling Is Associated with Clinical Outcome in Acute Ischemic Stroke Patients1Neurology, University of Southern California, Los Angeles, CA, United States, 2Neurosurgery, Beijing Tiantan Hospital, Capital Medical University, Beijing, People's Republic of China, 3Neurovascular Imaging Research Core and Department of Neurology, UCLA, Los Angeles, CA, United States, 4Neuro-Intensive Care Unit, Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People's Republic of China, 5Biomathematics, UCLA, Los Angeles, CA, United States, 6Neurology, UCLA, Los Angeles, CA, United States, 7Radiology, UCLA, Los Angeles, CA, United States
Synopsis
An automatic scoring system for assessing reperfusion status based on arterial spin labeled (ASL) perfusion MRI was developed and evaluated for acute ischemic stroke patients who received thrombolysis and/or endovascular treatment. Reperfusion injury is considered to have the same detrimental effects as non-reperfusion, and we applied the ASPECTS model to address the existence of heterogeneity of hypo- and hyper-perfusion despite vessel recanalization. Our newly devised reperfusion scoring system is highly associated with patient functional outcome and provides a useful tool to complement other clinical methods for managing corresponding strategies after treatment.
Purpose
In recent years, endovascular clot retrieval therapy has been introduced as an additional treatment option beyond the limited early time window for tPA in acute ischemic stroke (AIS) patients1,2. Despite excellent recanalization rate and subsequent reperfusion, favorable clinical outcomes are not as satisfactory as expected3. The hemodynamic status following successful recanalization is complex due to a variety of factors including heterogeneity of hypo- and hyper-perfusion, no reflow phenomenon, and reperfusion injury4, which all contribute to clinical outcome despite successful recanalization. The purpose of this study was to develop and evaluate a scoring system for assessing reperfusion status based on arterial spin-labeled (ASL) perfusion MRI in AIS patients receiving thrombolysis and/or endovascular treatment.Methods
The present study was performed on data collected from July 2010 to June 2014 in an ongoing prospective registry of patients evaluated with diffusion-perfusion MRI at an academic medical center. A total of 90 patients with unilateral AIS with proximal vascular occlusion in the anterior circulation who had undergone intravenous tPA and/or endovascular therapy were included. Pseudo-continuous ASL with background suppressed 3D GRASE was performed along with diffusion weighted imaging (DWI) within 24 hours after treatment on Siemens 1.5T Avanto or 3T TIM Trio systems using a 12-channel head coil. Quantitative cerebral blood flow (CBF) maps were calculated based on a previously published model5, co-registered with DWI, and normalized to the MNI template space using SPM8.
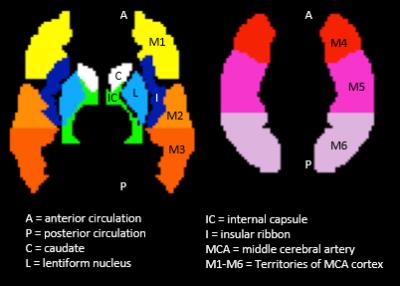
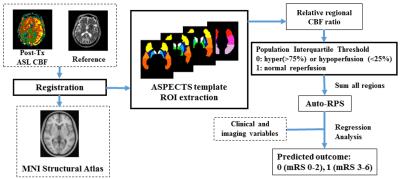
We devised an automatic reperfusion score (auto-RPS) based on the Alberta Stroke Program Early CT Score (ASPECTS) 10-point scale system6 to individually predict patient clinical outcome post-thrombolysis/endovascular treatment. Regional perfusion parameters in the 10 ASPECTS brain regions7 (Figure 1) were extracted from each hemisphere automatically from the CBF map in each patient using an in-house developed Matlab program. Relative ratio of CBF in the lesion region and its contralateral region was calculated. Because either hypo- or hyper-perfusion is related to bad outcome as reported in past studies8,9, points are deducted from 10 where hypo- or hyper-perfusion of a scored region warrants a point deduction. Based on our database of CBF measurements, hypo- and hyper-perfusion were tentatively defined as the 25th and 75th percentiles, respectively. The flow chart of the proposed scoring system is shown in Figure 2.
Two stroke fellows with ASPECTS training calculated manual-RPS on post-treatment ASL perfusion maps and DWI-ASPECTS based on post treatment DWI. In 48 cases, the recanalization status Thrombolysis in Cerebral Infarction (TICI) score was recorded, where TICI>2b is considered successful recanalization. Favorable outcomes were defined by a modified Rankin Scale score of 0-2 at 3 months after the occurrence of stroke. Statistical analysis was performed using SPSS and R. To evaluate the predictive value of auto-RPS, manual-RPS, DWI-ASPECTS, and TICI, the receiver operating characteristic (ROC) curve of the univariate logistic regression was constructed, and the area under the ROC curve (AUC) was used as a scalar measure to assess the performance of prognostic risk scores.
Results and Discussion
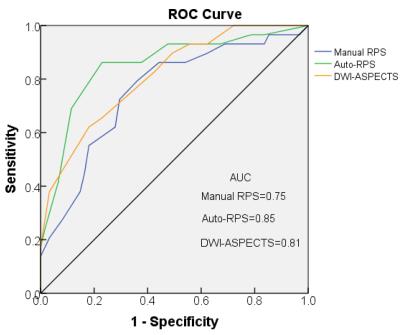
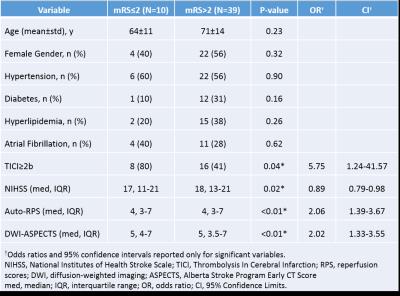
Auto-RPS correlated positively with DWI-ASPECTS (ρ=0.66, P<0.001) and was on average 1 point lower than DWI-ASPECTS (P<0.001). The ROCs and AUCs for predicting mRS functional outcome for all 90 cases are shown in Figure 3. There was no significant difference of AUC between manual RPS vs. auto-RPS (P=0.10), manual RPS vs. DWI-ASPECTS (P=0.4), and auto-RPS vs. DWI-ASPECTS (P=0.3) (DeLong method). In the 48 cases with known TICI scores, auto-RPS and TICI did not correlate well (ρ=0.27, P>0.05, Spearman test) and discordance between the two modalities is commonly observed. In univariate logistic regression analysis, auto-RPS (P<0.01), DWI-ASPECTS (P<0.01), TICI≥2b (P=0.04) and baseline NIHSS (P=0.02) were associated with favorable functional outcome at 3 months (Table 1). Using bi-directional stepwise multivariate logistic regression model selection, auto-RPS and TICI formed the best model fit. However, only auto-RPS emerged as a significant independent predictor of functional outcome (OR=2.06, 95% CI 1.39-3.67, P<0.01) in this multivariate model. Auto-RPS is on average 1 point lower than DWI-ASPECTS because auto-RPS is more sensitive than DWI-ASPECTS at detecting ischemic tissue changes. The discordance between the post-treatment auto-RPS and DWI-ASPECTS scores is described with example cases in Figure 4.Conclusion
The novelty of our study lies in the insight that reperfusion injury is considered to have the same detrimental effects as non-reperfusion (both warrant a point deduction), and we applied the ASPECTS model to address the existence of heterogeneity of hypo- and hyper-perfusion despite vessel recanalization. Our newly devised reperfusion scoring system is highly associated with patient functional outcome and provides a useful tool to complement other clinical methods for managing corresponding strategies after treatment.Acknowledgements
This study was supported by the US National Institutes of Health grant UH2NS100614.References
1. Kim D, Jahan R, Starkman S, et al. Endovascular mechanical clot retrieval in a broad ischemic stroke cohort. AJNR American journal of neuroradiology. 2006; 27: 2048-52.
2. Nesbit GM, Luh G, Tien R and Barnwell SL. New and future endovascular treatment strategies for acute ischemic stroke. Journal of vascular and interventional radiology : JVIR. 2004; 15: S103-10. 3. Goyal M. Poor clinical outcome despite successful arterial recanalization. What went wrong? How can we do better? Neuroradiology. 2010; 52: 341-3.
4. Nour M, Scalzo F and Liebeskind DS. Ischemia-reperfusion injury in stroke. Interventional neurology. 2013; 1: 185-99.
5. Wang DJ, Alger JR, Qiao JX, et al. The value of arterial spin-labeled perfusion imaging in acute ischemic stroke: comparison with dynamic susceptibility contrast-enhanced MRI. Stroke; a journal of cerebral circulation. 2012; 43: 1018-24.
6. Barber PA, Demchuk AM, Zhang J and Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000; 355: 1670-4.
7. Kretschmann H-J, Weinrich W and Kretschmann H-J. Cranial neuroimaging and clinical neuroanatomy : atlas of MIR imaging and computed tomography. 3rd ed. Stuttgart ; New York: Georg Thieme Verlag ; Thieme Medical Publishers, 2003, p.451 p.
8. Yu S, Liebeskind DS, Dua S, et al. Postischemic hyperperfusion on arterial spin labeled perfusion MRI is linked to hemorrhagic transformation in stroke. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2015; 35: 630-7.
9. Nour M, Scalzo F and Liebeskind DS. Ischemia-reperfusion injury in stroke. Interventional neurology. 2013; 1: 185-99.
Figures