0233
How Quick is our “Quick DWI” for Stroke?1Radiology, Royal Melbourne Hospital, University of Melbourne, Melbourne, Australia, 2Neurology, Royal Melbourne Hospital, University of Melbourne, Melbourne, Australia
Synopsis
Stroke is an emergency. Although MRI is the imaging gold standard for the ischemic “core” in the hyperacute setting, MRI must be “quick” to remain relevant in the management pathway of this common disease. A “quick diffusion weighted imaging”(qDWI) protocol for acute stroke consisting of a single DWI sequence was implemented at our institution. qDWI reduced scan time by 84% compared to our conventional “Stroke” protocol, was 96.5% diagnostic, and with 90% not requiring further MRI. There was also a statistically significant quicker referral to scan time compared to the conventional “Stroke” MRIs.
Clinical Question
Is there acute infarction—what tissue is dead?Impact
“Time is brain”—stroke is an emergency –early treatment improves clinical outcomes and reduces the economic costs of stroke associated long term disability1,2. Timely imaging diagnosis is imperative, and MRI needs to be “quick” to remain relevant in the management pathway of this disease that, worldwide, results in 1 death every 10 seconds, and an incidence of 1 every 2 seconds3. Although diffusion restriction on Diffusion-Weighted Imaging (DWI) is generally considered the imaging gold standard and superior to CT perfusion for the ischemic “core” in the hyper-acute setting4, 5, 6, MRI has largely been sidelined by CT in the selection of acute ischemic stroke patients for recanalization therapy due to CT’s ease of access and speed7, 8. Speedy diagnosis is not only needed for large territory proximal stroke potentially benefiting from endovascular therapy9, but also for lacunar strokes and transient ischemic attacks (TIA), with guidelines recommending imaging, preferably MRI, <24 hours of symptom onset10. TIAs confirmed to have diffusion restricting lesions are clinically reclassified and managed as stroke11. Speedy MRI is a challenge at multiple levels, but even if all other logistical hurdles are overcome, the scan time remains long, with a conventional “stroke” protocol requiring 20-30 minutes.
Approach
Our “Quick DWI”(qDWI) protocol consists of a single 2 minute 48 second DWI sequence after localizer (total scan time 3 minutes 7 seconds) with FOV 220mmx220mm, slice thickness 4mm (voxel size 1.3x1.3x4.0mm), TR 6160ms, TE 57ms, b-value 1000, EPI factor 58 and GRAPPA 2 (Aera, Siemens, Erlangen, Germany). This DWI sequence is from our “Stroke” protocol, which also has sagittal T1 MPRAGE, axial FLAIR/ T2 TSE/ SWI, and time of flight(TOF) MRA of the circle of Willis (total scan time 19 minutes 44 seconds).
The qDWI referral is made by stroke/neurology units to mainly answer 2 specific questions, with awareness of limitations: (1) Acute infarct? (2) Infarct volume? Size guides timing for starting anticoagulation. ((3) Any hemorrhage visible on qDWI is also useful information).
Gains and Losses
Broad anticipated gains:
1. Radiology
Quicker scan time: Easier to “slot in” qDWI at short notice, increase daily MRI scan throughput
Quicker reading/reporting/results
2. Stroke/neurology/emergency department (ED)
Quicker MRI access
Quicker diagnosis & decision making for treatment, risk assessment , timing of further investigations, admission/discharge
3. Hospital
More efficient scanner, bed and inpatient resource use
4. Patient
Quicker scans: less tissue radiofrequency energy deposition /discomfort/claustrophobia/motion
Quicker diagnosis/treatment with statistically better outcomes
Quicker discharge (for some)
Minimal anticipated losses:
1. DWI has high sensitivity (88-100%) and specificity (95-100%)10 for acute infarct, detectable within minutes of symptom onset, while T1, T2 and FLAIR are relatively insensitive for acute ischaemia10. However, negative DWI should raise possibility of underlying stroke mimic12, some easier to detect on other sequences (ie. FLAIR for multiple sclerosis).
2. DWI derived B0 images provide T2 weighted information
3. DWI using EPI readout provides T2* information, and can detect hemorrhage
4.
CT angiography
brain/neck, routinely part of stroke/TIA workup, provides the cerebro-vascular
information of MRA
Preliminary Data
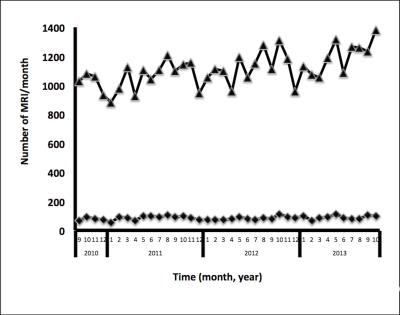
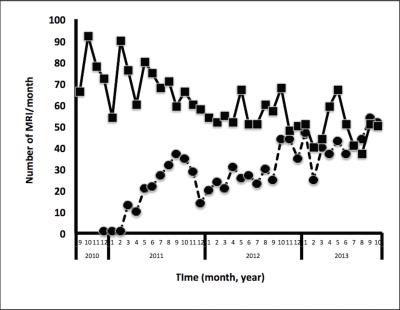
In our hospital, data from 1/12/2010 – 31/10/2013 show:
1. 280 hours stroke MRI scan time saved (=scan time for 5400 qDWI or 853 Stroke MRIs)
1013 qDWI and 2281 Stroke MRIs performed
17 minutes saved per qDWI (20 to 3 minutes, 84% reduction)
2. Total MRI for stroke workup stable (10% of all MRIs) Fig.1, but increased numbers of qDWI with decrease in Stroke MRIs to nearly 1:1 ratio by 2013 Fig.2
420(46%) qDWI and 491(54%) Stroke MRIs in 2013 (to October)
As ratio of qDWI to Stroke MRI increases, saved scan time increases: 116 hours saved in 10 months (=scan time for 2239 qDWI or 354 Stroke MRIs)
3. qDWI gave clear diagnosis in 977/1013 (96.5%)
Acute infarct 498(49.2%), no infarct 473(46.7%), subacute infarct 6(0.6%).
30(3%) equivocal, 2(0.2%) uninterpretable
4. 912/1013 (90%) qDWI patients did not have further MRI
No further imaging (Ultrasound/CT/MRI) 59%
Follow-up Stroke MRI 4%, other MRI 6%
Time to follow-up MRI (median[IQR]): Stroke protocol 12[4-59], other MRI 7[3-43], qDWI 4[1-7] days
Data from 18/8/2016 - 2/11/2016 show:
5. Quicker MRI access (referral to scan) time (median[IQR]): qDWI 0[0-1] and Stroke MRI 1[0.75-1.25] days, p=0.0017, Wilcoxon Mann-Whitney test
Total MRI for stroke workup 56: 44 qDWI versus 12 Stroke MRIs
70% qDWI performed on day of request versus 25% of Stroke MRIs
Conclusion
Our preliminary data show qDWI quick, frequently diagnostic and infrequently prompts further MR imaging.Acknowledgements
No acknowledgement found.References
1. Saver JL. Time is brain--quantified. Stroke. 2006;37(1):263-6.
2. Davis S, Lees K, Donnan G. Treating the acute stroke patient as an emergency: current practices and future opportunities. Int J Clin Pract. 2006;60(4):399-407.
3. Facts and Figures-World Stroke Campaign, 2016. Geneva, Switzerland: World Stroke Organization. http://www.worldstrokecampaign.org/learn/facts-and-figures
4. Copen WA, Morais LT, Wu O, et al. In acute stroke, can CT perfusion-derived cerebral blood volume maps substitute for diffusion-weighted imaging in identifying the ischemic core? PLoS One. 2015;10(7): e0133566.
5. Deipolyi AR, Wu O, Macklin EA, et al. Reliability of cerebral blood volume maps as a substitute for diffusion-weighted imaging in acute ischemic stroke. Magn Reson Imaging. 2012;36(5):1083-7.
6. Schaefer PW, Souza L, Kamalian S, et al. Limited reliability of computed tomographic perfusion acute infarct volume measurements compared with diffusion-weighted imaging in anterior circulation stroke. Stroke. 2015;46(2):419-24.
7. Lovblad K, Pereira VM. MRI of acute stroke: what went wrong? Am J Neuroradiol. 2015;36(11):1996-7.
8. Vymazal J, Rulseh AM, Keller J, et al. Comparison of CT and MR imaging in ischemic stroke. Insights Imaging. 2012;3(6):619-627.
9. Powers WJ, Derdeyn CP, Biller J, et al. 2015 AHA/ASA focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke. 2015;46(10):3020-35.
10. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke. Stroke. 2013; 44(3):780-947.
11. Sorensen AG, Hakan A. Transient ischemic attack definition, diagnosis and risk stratification. Neuroimaging Clin N Am. 2011;21(2):303-313.
12. Brunser AM, Hoppe A, Illanes S, et al. Accuracy of diffusion-weighted imaging in the diagnosis of stroke in patients with suspected cerebral infarct. Stroke. 2013;44:1169-1171.
Figures