0232
Faster and more accurate staging of rectal cancer through a two-sequence MR protocol based on high-resolution T1-weighted post-contrast 3D SPGR imaging1Dept. of Radiology, Stanford University, Stanford, CA, United States
Synopsis
A fast 10-min MRI protocol for rectal cancer staging based on a high-resolution T1-weighted post-contrast sequence was compared to a conventional 30-40 min protocol based on multiple planes of T2-weighted imaging. With IRB approval, 37 consecutive patients were retrospectively identified whose MRI rectal cancer staging studies contained the necessary sequences allowing creation of conventional and hypothetical fast protocols. Two blinded readers assessed each protocol for findings determining cancer stage. The fast 10-min MRI staging protocol was significantly more accurate for assessment of nodal disease and rectal cancer stage, and allowed significantly more confidence in assessment for transmural extension of tumor.
Purpose
Conventional MRI protocols for rectal cancer staging rely on multiple planes of T2-weighted (T2w) fast spin echo (FSE) imaging, with need for technologist skill to determine oblique planes, and with long total scan times (30-40 min)1. We investigated whether a fast 10-minute protocol based around a high-resolution free-breathing fat-suppressed post-contrast T1-weighted (T1w) 3D SPGR sequence (HiRes-SPGR) could potentially replace a conventional rectal MRI protocol.Methods
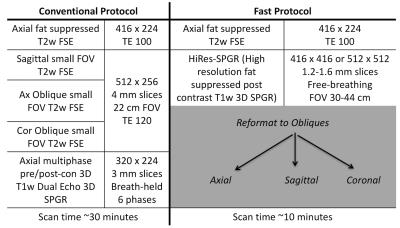
With IRB approval, we retrospectively identified 37 consecutive patients referred for 3T MRI staging of rectal cancer over a 23-month period whose studies contained all the necessary sequences (Figure 1). Rectal gel and intramuscular glucagon as a spasmolytic were administered immediately prior to the start of each scan.
Two readers (4 and 11 years of experience with body MRI) assessed in separate reading sessions either the conventional protocol (all sequences except the HiRes-SPGR), or a “fast” protocol consisting of only the HiRes-SPGR sequence plus the single fat-suppressed T2w sequence (Figure 1). Reading sessions were at least 3 months apart, and whether the conventional or the fast protocol was the initial protocol read was randomized.
Readers assessed imaging findings relevant to staging of rectal cancer, such as tumor penetration of the muscularis propria or invasion into adjacent pelvic structures, presence of nodal disease, and metastatic disease in the pelvis. A confidence measure from 1 (poor) to 4 (high) for the presence or absence of each finding was assessed. These reads were utilized to stage the tumor per AJCC guidelines2 for rectal cancer (35 cases), leiomyosarcoma (1 case), or rectal gastrointestinal stromal tumor (GIST, 1 case). For the gold standard, staging was derived from pathology reports if the patient went to surgery prior to other treatments, or from the clinically derived stage (reflecting a consensus of imaging results including PET/CT and endoscopic ultrasound when available as well as clinical findings) for those patients who underwent neoadjuvant therapy. Metastatic disease not included within the field of view of the MRI was ignored. The confidence score for T (primary tumor) and N (nodal) components of staging were calculated based off of the specific imaging feature that lead to the assessment. For incorrect assessments, the confidence was reassigned to a 1 for the purposes of comparison. Additionally, subjective image quality assessments of motion degradation, lesion margin delineation, lesion contrast, and ability to identify the mesorectal fascia were graded on a scale of 1 (non-diagnostic) to 4 (excellent) for the small field of view (sFOV) T2w sequences in the conventional protocol and the HiRes-SPGR sequence in the fast protocol. The null hypothesis of no significant difference was assessed with a two-tailed Wilcoxon sign-rank test with a p value ≤ 0.05 considered significant.
Results and Discussion
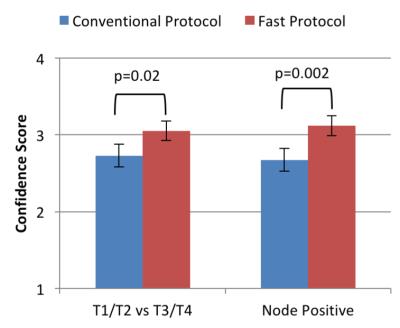
Confidence in assessment of transmural tumor involvement (T1/T2 vs T3/T4) and assessment of nodal involvement (N0 vs N1/N2) was significantly increased with the fast protocol (Figure 2). Accuracy of assessment of transmural tumor involvement was not significantly different with the fast protocol (correct in 84% of the fast protocol reads versus 72% of conventional protocol reads, p=0.07). Accuracy of assessment of nodal involvement was significantly increased with the fast protocol (correct in 84% of fast protocol reads, versus 68% of conventional protocol reads, p=0.008).
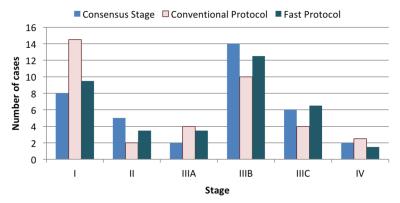
For overall staging, the fast protocol matched the final determined staging in 69% of cases versus 46% of cases evaluated with the conventional protocol (Figure 3), this difference was statistically significant (p=0.004). The differentiation between stage I, and stage II or greater disease, is the most clinically important result arising from MR based staging of rectal cancer, as this directly impacts whether patients are treated with initial surgery (stage I disease) or undergo neoadjuvant therapy (stage II or higher disease). With respect to deciding between stage I disease and stage II or greater disease, the fast protocol performed significantly better than the conventional protocol (88% correct versus 74%, p=0.019).
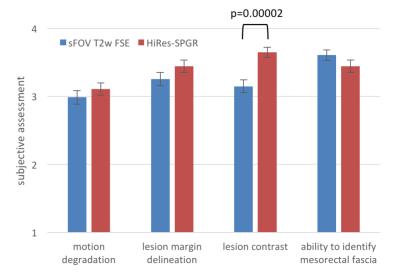
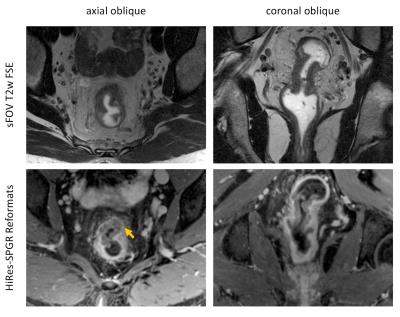
Assessment of subjective image quality measures showed a significant improvement in perceived lesion contrast with the HiRes-SPGR sequence (Figure 4). Motion degradation of imaging was rated similarly on the two protocols, which is expected as the HiRes-SPGR sequence requires similar acquisition time as a single FSE sequence. An example of the typical imaging appearance of rectal cancer with the two protocols is shown in Figure 5.
Conclusion
Compared to a conventional MRI protocol, a fast 10-minute MRI protocol for rectal cancer staging allowed greater reader confidence, and was more accurate for assessment of nodal disease and stage.Acknowledgements
This work was in part supported by NIH grant R01 EB009690. The authors would also like to thank the support of GE Healthcare.References
[1] Kaur H, et al., “MR Imaging for Preoperative Evaluation of Primary Rectal Cancer: Practical Considerations”, RadioGraphics 2012; 32:389-409.
[2] AJCC Cancer Staging Atlas: A Companion to the Seventh Editions of the AJCC Cancer Staging Manual and Handbook. Editors: Carolyn C. et al., 2012.
Figures