0230
5 Minute Comprehensive Knee MRI with 3D Double-Echo Steady-State (DESS)1Radiology, Stanford University, Stanford, CA, United States
Synopsis
Knee MRI is performed commonly in the US for assessing acute injuries as well as degenerative diseases. However, current knee MRI protocols can require 25-30 minutes or more and cost approximately $1.1billion/year. In such instances, a short knee protocol could lower costs while increasing patient throughput, comfort, and access to care. In this study, we show that a five-minute double-echo steady-state (DESS) scan, with automatic T2 maps and fluid-nulled images, offers high efficacy and diagnostic utility compared to the standard knee protocol. These results suggest that a five-minute DESS scan could be used for comprehensive MRI of the knee.
Clinical Question
Can 3D double-echo steady-state (DESS) be used as a highly sensitive and specific single-sequence five-minute knee protocol?Impact
Over 1 million people per year visit clinics in the US for acute knee injuries, for which MRI is commonly prescribed1. MRI is also commonly used to assess degenerative joint disorders, tumors, cysts, and general knee pain2. There are an estimated 200,000 ligament tears, 220,000 meniscal tears, and 6000 tendon ruptures per year in the US, while 63% of knee arthroscopies reveal chondral lesions3-6. Current knee MRI protocols can require 25-30 minutes or more and cost approximately $1.1billion/year in the US (assuming 1-hour scan blocks at $400/hour)7,8. In such instances, a five-minute knee protocol could lower costs while increasing patient throughput, comfort, and access to care9.Approach
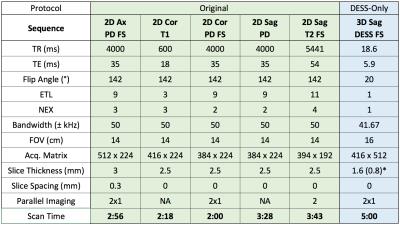
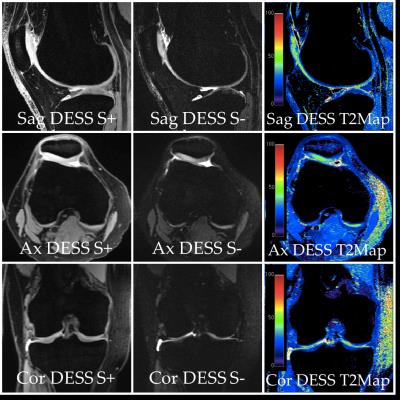
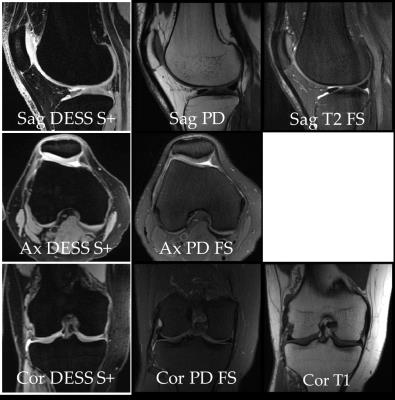
DESS generates two echoes, S+ (T1/T2-weighted) and S- (T2-weighted), which resemble proton-density and T2-weighting in the knee. A sum of the two signals can be used for cartilage morphometry (as in the Osteoarthritis Initiative) and a weighted subtraction creates fluid-nulled images10-12. More recently, it can be used for T2 measurements, which are created automatically and submitted to radiologist workstations at our institution immediately13-16. With these numerous contrasts (Figure 1), this study evaluated the feasibility of replacing the conventional knee protocol with a single five-minute DESS scan. Thus, water-only-excitation sagittal 3D DESS, with automatic axial and coronal reformatting, double-echo sum and subtraction, and T2 map generation, was added to the routine knee protocol (scan parameters and sample images in Table 1 and Figure 2). A secondary, exploratory goal of this study was to evaluate whether one additional sequence of the radiologist’s choosing, in conjunction with DESS, could be used for an abridged (<10 min) knee protocol (hereafter referred to as DESS+1 protocol).Gains and Losses
DESS provides morphological information and fluid-sensitivity, similar to a standard protocol, but with 3D-coverage and additional T2 maps and fluid-nulled images. While reformatting may obscure smaller structures such as the collateral ligaments, these injuries are often treated non-surgically, which does not change health management.Preliminary Data
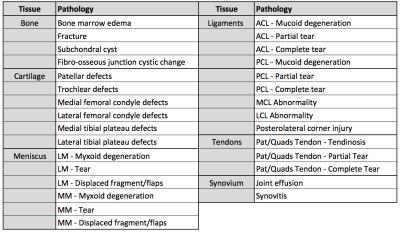
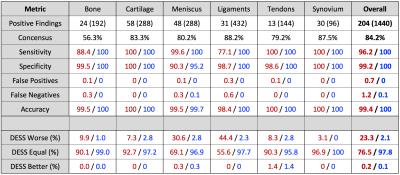
16 consecutive knee MRI patients were scanned following IRB-approved informed consent. 3 radiologists scored the scans for thirty abnormalities (sub-divided into bone, cartilage, meniscus, tendons, ligaments, and synovium in Table 2). The readers assessed the presence of pathologies (Yes/No) and subjectively scored the diagnostic utility provided by the protocol (0 = no utility, 1 = low utility, 2 = moderate utility, 3 = high utility). All readers first scored the DESS-only protocol, then chose the additional sequence to score the DESS+1 protocol, and then scored the original protocol.
Specificity, sensitivity, false-positives, false-negatives, and accuracy for the DESS and DESS+1 protocols were calculated, using the original protocol as the gold standard (Table 3). Consensus was established if all readers agreed on the presence/absence of the pathology. Diagnostic utility scores for DESS-only and DESS+1 protocols were compared to those of the original protocol (Table 3).
DESS had high sensitivity, specificity, and accuracy (Table 2) especially in the cartilage, menisci, tendons, and synovium. Cartilage abnormalities were well visualized in S+ and the T2 maps. For menisci and tendons, S+ outlined the morphology and a high S- signal indicated degeneration or tears. The fluid sensitivity allowed for accurate diagnoses of effusion and cysts. With proper training and more experience in a clinical knee-MRI population, T2 maps may additionally detect tears, mucoid and myxoid degeneration, and tendinosis.
DESS had lower ligament sensitivity (Table 3), largely due to the thin collateral ligaments being obscured in the reformatting. The robust fat suppression lowered contrast for delineating healthy (non-fluid surrounded) ligament boundaries and for diagnosing edemas. One reader exclusively scored menisci and ligaments as 2’s, however, this was a preference based on the high DESS signal, compared to routine scans, and did not affect DESS meniscal sensitivity. Imaging with slightly higher residual fat signals could enable better visualization of tissues at fatty interfaces and bony pathology. Additionally, acquiring twice as many slices in similar scan times with 2x2 parallel imaging (volunteer scan in Comparison 10), may increase ligament conspicuity and sensitivity to injury. The original protocol required 24±3 minutes for scanning. For the DESS+1 protocol, coronal PD FS was chosen for 67% of exams, so even if this protocol is chosen, patient throughput could be increased to ~20mins/knee from 35mins/knee (assuming 10 minutes for setup).
In conclusion, encouraging results were obtained in this preliminary study and we expect to improve accuracy with minimal protocol modifications. This suggests that a five-minute DESS scan, for a total scanner time of 15 minutes, may deliver high value for patients undergoing knee MRI.
Acknowledgements
Research support provided by NIH AR0063643, NIH EB002524, NIH AR062068, and GE Healthcare.References
1. Verma, Adarsh, et al. "The lateral view: a screening method for knee trauma." Academic radiology 8.5 (2001): 392-397.
2. Institute of Medicine of the National Academies Report. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research, 2011. The National Academies Press, Washington DC. (page 62).
3. American Academy of Orthopaedic Surgeons, July 2007, Anterior Cruciate Ligament Injury: Surgical Considerations (July 11, 2008)
4. Mordecai, Simon C., et al. "Treatment of meniscal tears: An evidence based approach." World journal of orthopedics 5.3 (2014): 233.
5. Verdano, Michele Arcangelo, et al. "Quadriceps tendon tear rupture in healthy patients treated with patellar drilling holes: clinical and ultrasonographic analysis after 36 months of follow-up." MLTJ Muscles, Ligaments and Tendons Journal 4.2 (2014): 194-200.
6. Falah, Mazen, et al. "Treatment of articular cartilage lesions of the knee." International orthopaedics 34.5 (2010): 621-630.
7. Rinck, P. What is the Organ Distribution of MRI Studies? The European Magnetic Resonance Forum – EMRF. (2005).
8. Organization for Economic Cooperation and Development, OECD Health Statistics. (2015).
9. Oei, Edwin HG, et al. "Costs and effectiveness of a brief MRI examination of patients with acute knee injury." European radiology 19.2 (2009): 409-418.
10. Bruder H, Fischer H, Graumann R, Deimling M. A new steady-state imaging sequence for simultaneous acquisition of two MR images with clearly different contrasts. Magnetic resonance in medicine 1988;7(1):35-42.
11. Redpath TW, Jones RA. FADE--a new fast imaging sequence. Magnetic resonance in medicine 1988;6(2):224-234. 12. Lee SY, Cho ZH. Fast SSFP gradient echo sequence for simultaneous acquisitions of FID and echo signals. Magnetic resonance in medicine 1988;8(2):142-150.
13. Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society 2008;16(12):1433-1441.
14. Welsch GH, Scheffler K, Mamisch TC, Hughes T, Millington S, Deimling M, Trattnig S. Rapid estimation of cartilage T2 based on double echo at steady state (DESS) with 3 Tesla. Magnetic resonance in medicine 2009;62(2):544-549.
15. Staroswiecki E, Granlund KL, Alley MT, Gold GE, Hargreaves BA. Simultaneous estimation of T(2) and apparent diffusion coefficient in human articular cartilage in vivo with a modified three-dimensional double echo steady state (DESS) sequence at 3 T. Magnetic resonance in medicine 2012;67(4):1086-1096.
16. Sveinsson B, Gold, G., Hargreaves, B. Quantification and artifact reduction from simple modeling of DESS signals. In: Proceedings of the 24th Annual Meeting of ISMRM, Singapore, Singapore 2016:p. 788.
Figures