0228
The use of MRI in the diagnosis of Chronic Thromboembolic Pulmonary Hypertension1Academic Radiology, The University of Sheffield, Sheffield, United Kingdom, 2Insigneo, Institute of In-Vivo Medicine, 3Medizinische Hochschule Hannover, Germany, 4Pulmonary Vascular Disease Unit, Sheffield Teaching Hospitals, United Kingdom
Synopsis
As surgical pulmonary endarterectomy significantly improves survival in patients with chronic thrombo-embolic pulmonary hypertension it is important to correctly identify patients. Using cardiopulmonary MRI it is possible to screen for the presence of chronic thombo-emboli in all cases who can tolerate MRI, reducing the requirement for SPECT (and therefore patient radiation exposure). The same scan can also predict the presence of pulmonary hypertension, and due to a high specificity we can reduce the reliance upon an invasive test (right heart catheterisation) by around 50%.
Clinical Question:
Can MRI diagnose chronic thromboembolic pulmonary hypertension (CTEPH).Impact:
It is important to correctly identify chronic thromboembolic pulmonary hypertension (CTEPH), as surgical pulmonary endarterectomy leads to a significant improvement in survival(1). The diagnosis is defined by mean pulmonary artery pressure (mPAP) ≥25mmHg at right heart catheterisation (RHC), in the presence of segmental defects, typically on single photon emission computed tomography (SPECT) perfusion, after >3 months effective anticoagulation(2). CTEPH most commonly results from incomplete lysis of an acute pulmonary embolus; organisation of the thrombus causes pulmonary vascular obstruction(3), ultimately leading to increased pulmonary arterial pressure, right ventricular dysfunction and failure. Untreated the prognosis is poor. The true impact of the disease is not known, but 2 years after survival from acute pulmonary embolism the cumulative incidence of CTEPH is reported as 3.8% (4).
Thus, non-invasive MRI-based screening tests for CTEPH would be of real clinical benefit through reducing the number of tests required and reducing radiation doses.
Approach:
The current gold-standard screening test for CTEPH is perfusion SPECT. This involves injection of Tc-99m labelled macro-aggregated albumin, so perfusion SPECT involves exposure to ionising radiation, (effective dose of 0.017mSv/MBq) (5). Further limitations of SPECT include attenuation of the signal by breast tissues and relatively long acquisition times leading to blurring in the region of the diaphragm. After screening for emboli with Q SPECT patients undergo right heart catheterisation, an invasive test with a 1 % serious complication rate(6), to measure the pulmonary arterial pressure to assess for the presence of pulmonary hypertension. Cardio-pulmonary MRI is emerging as an important tool for assessing the structure and function of the right ventricle and lungs in patients with pulmonary hypertension (7,8). Work submitted to ISMRM 2017 derived and evaluated a model for the prediction of mean pulmonary arterial pressure (mPAP) in 816 pulmonary hypertension patients. This model is based upon the ventricular mass index (right ventricular mass divided by left ventricular mass), systolic and diastolic pulmonary artery size and pulmonary arterial flow (figure 1). In a validation cohort of 408 cases of all forms of PH there was 100% specificity with an MR-predicted mPAP of >38.Gains and Losses:
The use of dynamic contrast enhanced MRI to screen for CTEPH has multiple potential clinical advantages. It has high sensitivity and avoids exposure to radiation which is necessary when screening using SPECT. It also reduces the number of investigations that the patient requires. In the same MRI sitting, lasting approximately 1 hour in total there will also be available imaging information on the structure and function of the right and left ventricles and pulmonary artery. Based on cardio-pulmonary-vascular imaging multiparametric regression model over half of cases that the patients have pulmonary hypertension, potentially avoiding the future need for RHC. One potential issue for the MR imaging may be related to patient factors, particularly claustrophobia, or movement if the patient is unable to lie still.Preliminary Data:
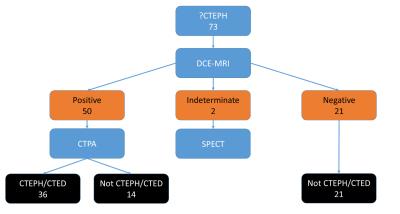
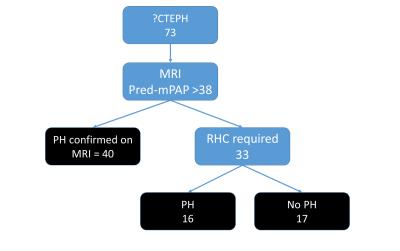
In a patient cohort of referrals to a national pulmonary hypertension centre with suspected CTEPH in 1 year from April 2013, we have 73 cases: 36 with CTEPH, 10 with CTED (chronic thromboembolic disease but with no pulmonary hypertension) and 27 with no CTEPH or CTED. Of the no CTEPH/CTED category 6 had no PH and 21 had PH due to other causes. There were 2 indeterminate DCE-MRI scans, which would require screening with SPECT. In all of the other cases we could replace nuclear medicine SPECT imaging with MRI. With the mPAP predictive algorithm we can also predict the presence of PH. Using a cut-off of predicted mPAP ≥38 mmHg we would be able to avoid right heart catheterisation 39 patients of the 73 total as MRI confirms that they have PH. This would represent a significant reduction in the workload of the PH department, with its associated potential money saving. From a patient perspective a reduction in the need for an invasive test and radiation exposure is valuable. The flow of patients through this ‘pathway’ is shown in figure 1 and 2. Once the patients have a positive DCE-perfusion MRI they would require a CTPA to confirm the presence of emboli and to assess for surgical accessibility. Further work will concentrate on increasing the accuracy of the predictive equation, particularly in differentiating the normal patients from the mild pulmonary hypertension patients (improving specificity). A combination of DCE-MRI and CMR prediction of mPAP avoids the requirement for SPECT imaging in all patients that can tolerate MRI and could potentially significantly reduce the number of right heart catheterisation procedures that are required, by at least 50%.Acknowledgements
This work presents independent research funded by the National Institute for Health Research (NIHR) and the MRC. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.References
1. Delcroix M, Lang I, Pepke-Zaba J, Jansa P, D’Armini AM, Snijder R, et al. Long-Term Outcome of Patients with Chronic Thromboembolic Pulmonary Hypertension?: Results from an International Prospective Registry. Circulation. 2016;133(9):859–71.
2. Wilkens H, Lang I, Behr J, Berghaus T, Grohe C, Guth S, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): Updated Recommendations of the Cologne Consensus Conference 2011. Int J Cardiol [Internet]. Elsevier Ireland Ltd; 2011;154(1):S54–60. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0167527311704934
3. Auger WR, Kim NH, Trow TK. Chronic thromboembolic pulmonary hypertension. Clin Chest Med [Internet]. 2010 Dec [cited 2015 Oct 13];31(4):741–58. Available from: http://www.sciencedirect.com/science/article/pii/S0272523110000870
4. Pengo V, Lensing AWAA, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of Chronic Thromboembolic Pulmonary Hypertension after Pulmonary Embolism. N Engl J Med [Internet]. 2004 May 27 [cited 2015 Oct 13];350(22):2257–64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15163775
5. Bajc M, Neilly JB, Miniati M, Schuemichen C, Meignan M, Jonson B. EANM guidelines for ventilation/perfusion scintigraphy?: Part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging. 2009;36(8):1356–70.
6. Hoeper MM, Lee SH, Voswinckel R, Palazzini M, Jais X, Marinelli A, et al. Complications of Right Heart Catheterization Procedures in Patients With Pulmonary Hypertension in Experienced Centers. J Am Coll Cardiol [Internet]. 2006 Dec;48(12):2546–52. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0735109706023382
7. Rajaram S, Swift AJ, Capener D, Telfer A, Davies C, Hill C, et al. Diagnostic accuracy of contrast-enhanced MR angiography and unenhanced proton MR imaging compared with CT pulmonary angiography in chronic thromboembolic pulmonary hypertension. Eur Radiol [Internet]. 2012;22(2):310–7. Available from: http://link.springer.com/10.1007/s00330-011-2252-x
8. Schoenfeld C, Hinrichs J, Renne J, Olsson KM, Gutberlet M, Welte T. MR Imaging – derived Regional Pulmonary Parenchymal Perfusion and Cardiac Function for Monitoring Patients with Pulmonary Hypertension before and after Pulmonary. Radiology [Internet]. 2016;0(0):1–10. Available from: http://pubs.rsna.org/doi/abs/10.1148/radiol.2015150765