0227
Contrast-enhanced Ultrashort Echo Time (UTE) MR of the chest to evaluate for metastatic nodules in pediatric patients with malignancy undergoing abdomen MR staging and surveillance: a high-value alternative or adjunct to CT1Radiology, Stanford University, Stanford, CA, United States
Synopsis
Ultrashort Echo Time (UTE) MRI of the chest can be optimized for detection of metastatic lung nodules. In pediatric patients with a history of abdominal malignancies undergoing routine re-staging contrast-enhanced MRI exams, clinically significant metastatic lung nodules are detectable which, if diagnosed, could obviate or decrease the frequency of subsequent separate CT scans of the chest. Though cost of a chest CT is lower than an MRI, it is substantially more than the incremental cost of adding an additional sequence during already-scheduled MR Abdomen exams. Additionally, ionizing radiation is avoided, alleviating concerns about cumulative exposure following multiple serial follow-up examinations.
Clinical Question:
In pediatric patients with a history of abdominal malignancies undergoing routine re-staging contrast-enhanced MRI exams, are clinically significant metastatic lung nodules detectable, which if diagnosed could obviate or decrease the frequency of subsequent separate CT scans of the chest?
Impact:
Malignancies account for a significant burden of pediatric disease, with prevalence of cancer among patients under 20 years age as high as 1.24 per 10001,2. Imaging plays an important role for staging the initial extent of disease or excluding recurrence, with multiple serial follow-up examinations.
For most tumors, MRI is the modality of choice for the abdomen and pelvis, but a separately scheduled CT Thorax exam is needed for the lungs, and radiation dose from serial CT exams is high. Also, exams are often performed under anesthesia, requiring MR to CT scanner transfer, which is lengthy, adding to risk. UTE MRI of the chest can be optimized for detection of metastatic lung nodules, and obtained during the staging MR Abdomen exam itself. Though the cost of a chest CT is marginally lower than MRI, it is substantially more than the incremental cost of adding an additional sequence during an already-scheduled MR exam.
Approach:
We performed UTE MRI as a single final sequence of our exam, and was thus contrast-enhanced (either ferumoxytol or Gadolinium-based agents). In our protocol, 320 x 320 matrix with FOV adjusted to patient size, 2 mm slices, TE 0.32 ms, and TR ~5 ms was used. We implemented a Self-Navigated Golden-Angle Ordered UTE sequence which utilizes conical sampling and echo times <0.1 ms that can image lung tissue with short relaxation times. This technique has a diffuse distribution of motion artifact, rendering images relatively robust to flow and motion.Gains and Losses:
From a clinical standpoint, the most significant gain is decreased duration of anesthesia since currently the entire transfer from CT to MRI is done in a sedated state, and the transfer time is much longer than the additional 5 minutes of MRI scanning of the chest. Next, ionizing radiation is avoided. Additionally, our method gains information regarding contrast enhancement, which may have some value in evaluating pulmonary nodules, but also results in improved characterization of the hilum and mediastinum, allowing evaluation of enhancing structures such as lymph nodes. For MRI exams with a concurrent abdomen, contrast is necessarily administered for tumor staging, whereas for thorax CT optimized for nodule surveillance, scans typically lack contrast. Assessment of pulmonary pathology such as differentiating between atelectasis and consolidation, or detecting pleural effusions, would be preserved and may even be enhanced, compared to CT. The clinician would likely lose information regarding small nodules under 5mm, although nodules smaller than 5mm are unlikely to be malignant in any patient population.3,4Preliminary Data:
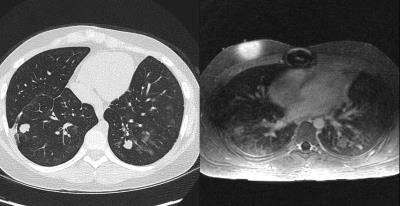
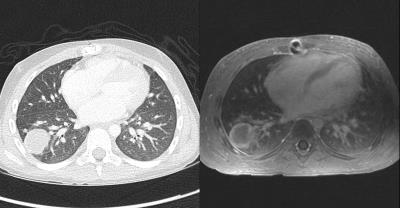
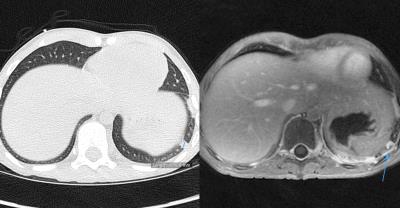
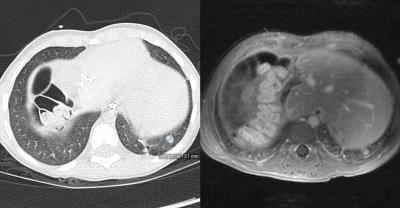
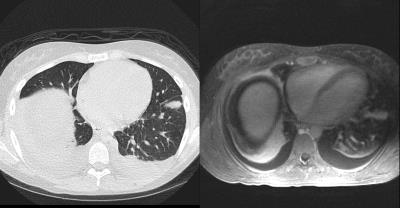
The diagnostic capability of UTE sequences is demonstrated by several paired images, where features of lung anatomy greater than 5mm such as nodules are clearly depicted. In some cases, additional lung pathologies such as effusions, consolidations and atelectasis may be better visualized than on CT.
Implementation of UTE MR Chest sequences may at least allow optimization of scheduling of the subsequent CT. For example, the chance discovery of a new nodule on MR could allow for an expedited CT scan, avoiding intangible costs of delayed diagnosis of distant metastatic disease. In addition, a baseline MRI at the time of CT could help determine which nodules are visible by both modalities, perhaps allowing decreased frequency of CT in favor of MR, analogous to alternating mammography/MRI screening strategies for high-risk breast cancer patients.
Price variation for MR studies varies widely, ranging between $300 to $3000 within a given geographic area.5,6 However technical costs can be modeled more reliably. In a comparison of true technical costs of MRI and CT, a linear cost per minute for MR was determined at $3.13/min.7 Under this paradigm, the marginal increase of a projected 4 minute contrast-enhanced dedicated UTE sequence on an Abdominal MRI would be relatively minor. Accordingly, the cost of abdominal contrast-enhanced MRI including chest UTE would be approximately $118. This is about half the cost of current care ($205): abdominal contrast-enhanced MRI of $106 and a 5-minute CT with contrast of $99.
Finally, radiation-dose savings should noted. The use of chest UTE MR to minimize chest CT in pediatric populations supports Society of Pediatric Radiology Image Gently® initiatives. In addition, despite new strategies for dose reduction, parents express evermore frequent concern about radiation exposure, sometimes even leading to underdosed, delayed, or cancelled CT exams, potentially leading to suboptimal outcomes. A chest MRI strategy would be a ready alternative.
Acknowledgements
No acknowledgement found.References
1. Kaatsch, Peter. "Epidemiology of childhood cancer." Cancer treatment reviews 36.4 (2010): 277-285.
2. Hewitt, Maria, Susan L. Weiner, and Joseph V. Simone, eds. Childhood cancer survivorship: improving care and quality of life. National Academies Press, 2003.
3. Burris, Nicholas S., et al. "Detection of small pulmonary nodules with ultrashort echo time sequences in oncology patients by using a PET/MR system." Radiology 278.1 (2015): 239-246.
4. Hanamiya M, Aoki T, Yamashita Y, Kawanami S, Korogi Y. Frequency and significance of pulmonary nodules on thin-section CT in patients with extrapulmonary malignant neoplasms. Eur J Radiol 2012;81(1):152–157. CrossRef, Medline
5. Wu, Sze-jung, et al. "Price transparency for MRIs increased use of less costly providers and triggered provider competition." Health Affairs 33.8 (2014): 1391-1398.
6. Fletcher, J., et al. "The cost of MRI: changes in costs 1989-1996." The British journal of radiology 72.857 (1999): 432-437.
7. Alex Lewis, Andreas Loening, and Shreyas Vasanawala. Comparison of True Technical Costs of MRI and CT. Abstract 1628. Proc. Intl. Soc. Mag. Reson. Med. 23 (2015).
Figures