0226
Demonstrating the Clinical Feasibility of a Rapid Non-Contrast MRI Protocol for Detection and Quantification of Hepatic Steatosis and Iron Overload1University of Wisconsin, Madison, WI, United States
Synopsis
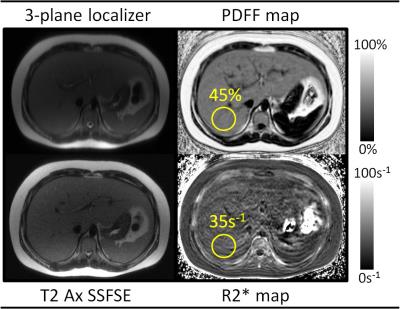
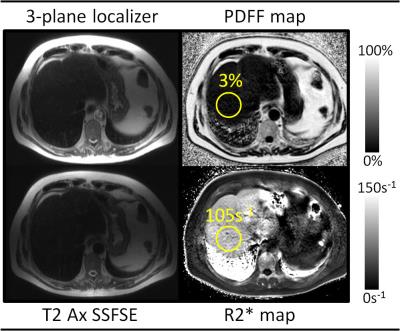
Many clinical scenarios necessitate evaluation for hepatic steatosis or iron overload without indication for a complicated MR exam. Emerging confounder-corrected chemical shift encoded MRI (CSE-MRI) techniques can provide simultaneous estimation of liver proton density fat fraction (PDFF) and R2* as biomarkers of steatosis and iron overload, respectively. We have developed a highly focused CSE-MRI protocol which obtains these metrics in approximately 5 minutes of table time. Our initial clinical experience has shown this protocol to be feasible for evaluation of patients ranging from pediatric to geriatric, with clinically significant disease detected in a large fraction of patients scanned to date.
Introduction
In many clinical situations, there is a specific clinical question to determine the presence and severity of hepatic steatosis and/or iron overload without the need for a lengthy MR exam. Emerging confounder-corrected chemical shift encoded MRI (CSE-MRI) techniques can provide accurate and precise biomarkers of liver fat [1] and iron concentration [2]. Within a single short breath-hold, these methods can provide simultaneous estimation of the proton density fat fraction (PDFF) and R2*, as biomarkers of hepatic steatosis and liver iron overload, respectively.
Our institution developed and validated an FDA-approved single breath-hold CSE-MRI method of simultaneous quantification of tissue triglyceride concentration and iron overload, and implemented it into a limited, rapid protocol, hereafter referred to as the "rapid fat/iron protocol". The rapid fat/iron protocol requires patients to hold their breath for a total of three 20-second intervals and can be completed in approximately 5 minutes of table time.
This protocol provides two main quantitative metrics: liver proton density fat fraction (PDFF, %), which serves as an imaging biomarker of liver fat content, and R2* (s-1), which represents the rate of decay of the MR signal and is linearly related to liver iron concentration [3].
Purpose
To demonstrate the feasibility of a rapid fat/iron protocol based on CSE-MRI for detection and quantification of hepatic steatosis and iron overload in the clinical setting.Methods
We retrospectively reviewed the imaging examinations and medical records of patients at our institution undergoing the rapid fat/iron protocol from April 2014 through October 2016. We collected and recorded patient demographic information (including age and sex), exam indication, exam time, and exam results (PDFF and R2*) as reported by the interpreting radiologist. These data were collated and analyzed.Results
A total of 51 rapid fat/iron protocol examinations from 45 patients were identified. Mean [±SD] patient age was 23.2 ± 23.8 years (range, 8-72 years), including 29 males and 16 females. 21 patients were under the age of 18. Six patients underwent two scans during the study period, while the remaining39 patients underwent one scan each. All patients who underwent two scans were children, with a range of 8-13 years at the time of initial scan.
Indication for rapid fat/iron protocol MRI was evaluation for hepatic steatosis in N=26 scans, evaluation for iron overload in N=19 scans, and evaluation of nonspecific elevated liver function tests (LFTs) in N=6 scans. Indications for patients under 18 years of age (N=27 scans) were hepatic steatosis in N=22 scans and elevated LFTs in N=5 scans. In patients 18 and over (N=24 scans), indications were hepatic steatosis in N=4 scans, iron overload in N=19 scans, and elevated LFTs in N=1 scan.
Mean table time for rapid fat/iron protocol MRI scans was 6.8±3.2 minutes (range, 2-17 minutes) with a median table time of 6 minutes. 39 scans were performed on 1.5T scanners and 12 scans were performed on 3T scanners. In no patient, including children, was anesthesia or sedation used.
In patients for whom the scan indication was hepatic steatosis (N=26), the mean PDFF was 24.6±11.1% (normal liver PDFF <5%) with a range of 3-50%. Liver PDFF was <5% in only 1/26 of these scans. In patients for whom the scan indication was iron overload (N=19), the mean R2* was 76.9±96.7s-1 (range, 25-415s-1) for scans performed at 1.5T (N=15, normal liver R2* <60s-1) and 124.4±58.2s-1 (range 89-203s-1) for scans performed at 3.0T (N=4, normal liver R2* <120s-1). R2* was abnormally high in 7/19 scans performed for iron overload. All patients who were scanned for nonspecific elevated LFTs (N=6) had abnormally high liver PDFF (mean 24.2±7.7%) with normal R2* values.
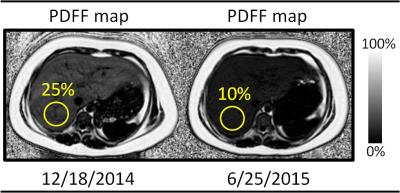
Six patients underwent two rapid fat/iron studies for treatment monitoring of hepatic steatosis. These studies occurred a mean of 436±112 days apart. PDFF decreased by an average of 8.9±11.3% during the follow-up interval. Only one patient saw an increase in liver PDFF during this time.
Discussion
Our clinical experience shows that focused MRI evaluation for hepatic steatosis or iron overload using the rapid fat/iron protocol can be performed with a median table time of 6 minutes. This protocol has been used in patients ranging in age from 8 to 72 years, without the need for anesthesia or sedation in children. Abnormally elevated liver PDFF or R2* was detected in a large majority of patients, indicative of possible under-utilization or other patient selection issues.Conclusion
Focused MRI examinations for specific clinical indications, such as this protocol for detection and quantification of hepatic steatosis and iron overload, are feasible in busy clinical practice.Acknowledgements
No acknowledgement found.References
1. Reeder SB, Cruite I, Hamilton G, Sirlin CB. Quantitative Assessment of Liver Fat with Magnetic Resonance Imaging and Spectroscopy. J Magn Reson Imaging 2011 Oct;34(4):729-49
2. Hernando D, Levin YS, Sirlin CB, Reeder SB. Quantification of Liver Iron with MRI: State of the Art and Remaining Challenges. J Magn Reson Imaging 2014 Nov;40(5):1003-21.
3. Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD. MRI R2 and R2* Mapping Accurately Estimates Hepatic Iron Concentration in Transfusion-Dependent Thalassemia and Sickle Cell Disease Patients. Blood 2005;106(4):1460-65.
Figures