0225
Diagnostic performance of an abbreviated gadoxetic acid enhanced-MRI (AMRI) vs. ultrasound for detection of small HCC: pilot study.1Translational and Molecular Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2Radiology, Groupe Hospitalier Pitié Salpêtrière, Paris, France, 3Department of Medicine/Division of Liver Diseases, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4Radiology, Division of Abdominal Radiology, University of Michigan Health System, Ann Arbor, MI, United States, 5Liver Imaging Group, Department of Radiology, University of California, San Diego, CA, United States
Synopsis
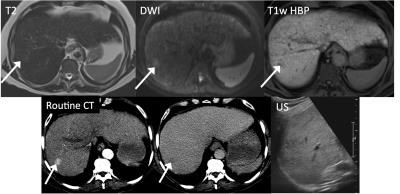
In this study, we aim to test the diagnostic value of an abbreviated MRI (AMRI) using gadoxetic acid (with patient injected outside the MRI room) compared to ultrasound (US) for hepatocellular carcinoma (HCC) detection in a population of patients with small HCC and controls. This study demonstrates that AMRI using T1WI obtained at the hepatobiliary phase (T1w-HBP), diffusion weighted imaging (DWI) and T2WI has superior diagnostic performance for HCC detection compared to US. This could serve as the basis for a future study assessing AMRI for HCC screening/surveillance in patients with cirrhosis.
Purpose
Current state-of-the-art liver MRI using T1WI obtained at the hepatobiliary phase (HBP) obtained after gadoxetic acid with [1, 2] or without [3-6] diffusion-weighted imaging (DWI) has been shown recently to yield improved sensitivity for detection of small hepatocellular carcinoma (HCC). However, there are some disadvantages of MRI including exam length and cost, for instance compared to ultrasound (US) and CT. An abbreviated MRI (AMRI) protocol with gadoxetic acid contrast injected outside the room, combining only T1-HBP, DWI and T2 HASTE may reduce costs associated with MRI, and may ultimately benefit patients at risk for HCC as it could be used for screening. In this study, we aim to compare the diagnostic performance of an AMRI protocol compared to US for the detection of small (<2 cm) HCC in a population of cirrhotic patients. Methods
19 patients with cirrhosis and known HCC ≤ 2 cm and controls (M/F 14/5, mean age 57 y) who underwent AMRI and liver US in the same day for HCC detection were included in this IRB approved prospective single-center study. AMRI liver protocol was performed in a 1.5T system (Siemens Aera) and consisted in injection of a standard dose of 0.025 mmol/Kg of gadoxetic acid (Eovist/Primovist, Bayer) outside the MRI room so that patient is scanned in one session during the peak hepatocyte uptake, with no dynamic contrast-enhanced T1WI obtained. AMRI protocol (≤15 min) included axial T2w HASTE, free breathing DWI and axial T1w- HBP (2 BH). US were performed by dedicated US technicians that were blinded to prior imaging studies. Two independent radiologists (Obs.1 and 2) assessed 2 sets of images (non-contrast AMRI: DWI + T2w and AMRI: T1w-HBP+ DWI + T2w) to detect liver lesions (≥1cm) using the following criteria: 1=negative (no lesions), 2=benign (cyst or hemangioma) and, 3= positive (suspicious lesion, not cyst or hemangioma). A patient was considered as test positive when readers designated a score of 3 (positive study) for AMRI and/or US. Reference standard was represented by consensus interpretation of 2 separate readers using OPTN criteria using full contrast-enhanced MRI or CT obtained separately. Per patient sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated in terms of concordance between the classification of patients as positive versus negative at reference standard and the classification of patients as test-positive versus test-negative for a given combination of reader and imaging features for AMRI and US.Results
10 initial patients with 12 HCCs (15.2 ± 0.3 mm) and 9 patients without HCC (controls) were analyzed and are reported. Diagnostic performance for non-contrast AMRI, AMRI and US are shown in Table 1. Higher per-patient sensitivity and NPV were observed for AMRI (Fig.1). AMRI showed higher accuracy compared to non-contrast AMRI and US. Substantial interreader agreement was found for non-contrast AMRI and AMRI (kappa of 0.62 and 0.7 respectively).Discussion and Conclusion
This pilot study demonstrates that AMRI has superior diagnostic performance for HCC detection compared to US. There is limited data on the diagnostic performance of HCC detection using an AMRI protocol, with no published data comparing this imaging approach to US. Recent studies have shown that AMRI has a clinically acceptable sensitivity and NPV for HCC detection when compared to dynamic contrast-enhanced (CE)-T1w imaging [7-9], with authors concluding that an AMRI may be an acceptable lower cost alternative to a standard dynamic MRI for HCC surveillance in the setting of chronic liver disease at centers that rely on MRI for examination. This study will help define and validate a novel, rapid, accurate, and potentially cost-effective imaging protocol for HCC screening in high-risk individuals.Acknowledgements
No acknowledgement found.References
1. Park, M.J., et al., Small hepatocellular carcinomas: improved sensitivity by combining gadoxetic acid-enhanced and diffusion-weighted MR imaging patterns. Radiology, 2012. 264(3): p. 761-70.
2. Lee, M.H., et al., Gadoxetic acid-enhanced hepatobiliary phase MRI and high-b-value diffusion-weighted imaging to distinguish well-differentiated hepatocellular carcinomas from benign nodules in patients with chronic liver disease. AJR Am J Roentgenol, 2011. 197(5): p. W868-75.
3. Ahn, S.S., et al., Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology, 2010. 255(2): p. 459-66.
4. Sano, K., et al., Imaging study of early hepatocellular carcinoma: usefulness of gadoxetic acid-enhanced MR imaging. Radiology, 2011. 261(3): p. 834-44.
5. Di Martino, M., et al., Intraindividual comparison of gadoxetate disodium-enhanced MR imaging and 64-section multidetector CT in the Detection of hepatocellular carcinoma in patients with cirrhosis. Radiology, 2010. 256(3): p. 806-16.
6. Kim, S.H., et al., Gadoxetic acid-enhanced MRI versus triple-phase MDCT for the preoperative detection of hepatocellular carcinoma. AJR Am J Roentgenol, 2009. 192(6): p. 1675-81.
7. Besa, C., et al., Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdom Radiol (NY), 2016.
8. Marks RM, R.A., Heba ER, Tang A, Wolfson TJ, Gamst AC, Sirlin CB, Bashir MR, Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR Am J Roentgenol. , 2015. 204(3): p. 527-35.
9. Kim, Y.K., et al., Noncontrast MRI with diffusion-weighted imaging as the sole imaging modality for detecting liver malignancy in patients with high risk for hepatocellular carcinoma. Magn Reson Imaging, 2014. 32(6): p. 610-8.
Figures