0222
Cost-Utility Analysis of Ultrasound, Computed Tomography, Abbreviated and Standard MRI for Hepatocellular Carcinoma Surveillance1Radiology, University of Montreal, Montreal, QC, Canada, 2Centre de recherche du Centre hospitalier de l'Université de Montréal (CRCHUM), Montreal, QC, Canada, 3Gastroenterology and Hepatology, University of Montreal, Montreal, QC, Canada, 4Health Technology Assessment Unit, 5Faculty of Pharmacy and Pharmacoeconomics, University of Montreal, Montreal
Synopsis
Current clinical practice guidelines recommend ultrasound (US) every 6 months for surveillance of hepatocellular carcinoma (HCC) in at-risk patients. Despite higher sensitivity, there is uncertainty regarding the role of MRI for HCC surveillance, whether as an add-on or replacement test. Our results indicate that surveillance with standard MRI followed by CT if technically inconclusive provided the highest level of effectiveness. However, CT followed by MRI was more cost-effective than alternative surveillance strategies using a threshold of $50,000 per QALY gained. Further, lower cost of abbreviated MRI will be required to be used as a first-line imaging technique for surveillance.
Introduction
Current clinical practice guidelines recommend ultrasound (US) every 6 months for surveillance of hepatocellular carcinoma (HCC) in at-risk patients.1,2 While US surveillance is feasible in "echogenic" patients with thin body habitus or without steatosis, it is challenging in large, steatotic or cirrhotic patients.3 Further, prior cost-effectiveness studies on US-based surveillance have not taken into account the possibility of technically inconclusive imaging examinations.
Hence, we explored the cost-effectiveness of no surveillance and 7 imaging-based strategies which accounted for technically inconclusive, negative, and positive studies in at-risk patients. We also performed a sensitivity analysis to identify the key drivers of cost-effectiveness for a surveillance strategy based on abbreviated MRI.
Method
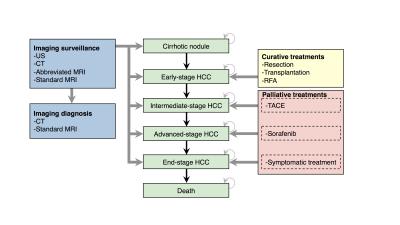
We performed a cost-utility analysis of 6-month non-invasive surveillance strategies using a third-party payer perspective in patients at risk for HCC. A decisional Markov model was developed to estimate the expected costs and quality-adjusted life years (QALYs) associated with surveillance strategies for HCC. This model was constructed to reflect the imaging-based approach to HCC surveillance and diagnosis and to mirror the treatment options favored for each HCC disease stage, as advocated by the American Association for the Study of Liver Diseases (AASLD) practice guidelines (Figure 1).2
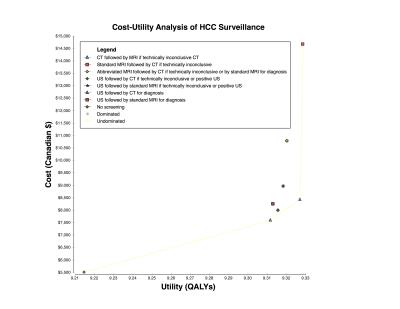
We investigated various surveillance strategies which relied on combinations of imaging techniques: US, contrast-enhanced CT, abbreviated MRI, and standard MRI (Figure 2).4 Contrast-enhanced CT and standard MRI were compared as confirmation methods whenever surveillance techniques were not technically inconclusive. Canadian dollar (C$) costs were adjusted for inflation and discounted at 5%. Costs, QALYs, and incremental cost-effectiveness ratios (ICER) were calculated using no surveillance as the base comparator. We used a willingness-to-pay threshold of C$50,000/QALY.
Results
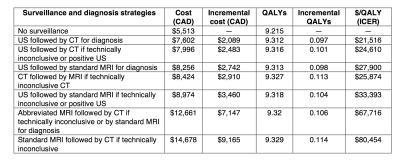
Table 1 summarizes each surveillance strategy with associated costs, QALYs and ICERs using no surveillance as the common baseline. The cost-utility results are illustrated in Figure 3.
Compared with no surveillance, surveillance with CT followed by MRI for technically inconclusive CT had an ICER of C$ 25,874 per QALY gained; surveillance with US followed by standard MRI for technically inconclusive or positive US had an ICER of C$ 33,393; surveillance with abbreviated MRI followed by CT for a technically inconclusive study or by standard MRI for diagnosis had an ICER of C$ 67,716. Surveillance with standard MRI followed by CT if technically inconclusive was the most effective but also the most expensive strategy, with an ICER of C$ 80,454.
One-way sensitivity analysis for surveillance with abbreviated MRI vs. no screening is summarized in Figure 4. The three parameters that had the greatest effect on the ICER were the transition probability from cirrhosis to HCC, the cost of abbreviated MRI, and cost of a hepatectomy. The ICER respected the willingness-to-pay threshold if the cost of abbreviated MRI was lower than C$ 211 per examination.
Discussion
1) Our model suggests that, in a high-risk population, surveillance strategies that used standard MRI, abbreviated MRI, or CT as a first-line modality were the most effective. However, only CT followed by MRI for technically inconclusive results was more cost-effective than alternative surveillance strategies using a threshold of $50,000 per QALY gained.
2) Our results, which incorporate estimates of diagnostic accuracy from recent meta-analyses of US, CT, and MRI5,6 and from the simulation of an abbreviated MRI protocol for detection or diagnosis of HCC,4 indicate that MRI as a first-line modality was the most effective strategy, although not cost-effective. These results are consistent with those of a prior cost-effectiveness study which compared these imaging modalities.7
3) From the perspective of a universal healthcare system, surveillance strategies based on abbreviated or standard MRI as first-line modalities exceeded the willingness-to-pay threshold generally accepted in Canada.
4) Adoption of MRI as a surveillance modality would require a paradigm shift from a diagnostic study with low volume, high accuracy, and long acquisition time to a surveillance study with high volume, high sensitivity, and short acquisition time.
5) Our micro-costing simulations suggest that consistently shorter exam duration (≤ 5 min) and lower total cost per unit —including contrast agent, supplies, and professional fees for interpretation— will be required to become cost-effective.
Conclusion
Our model suggests that HCC surveillance in high-risk patients with standard MRI or abbreviated MRI as first-line modalities are among the most effective, but are not cost-effective at the current willingness-to-pay threshold generally accepted by the Canadian healthcare system. To become cost-effective, HCC surveillance with abbreviated MRI would require innovative approaches to lower total examination cost and shorten examination time.Acknowledgements
An Tang is supported by a Career Award from the Fonds de recherche du Québec en Santé and Association des Radiologistes du Québec (FRQS-ARQ #26993) and a New Researcher Startup Grant from the Centre de Recherche du Centre Hospitalier de l'Université de Montréal (CRCHUM).References
1. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43.
2. Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020-2.
3. Choi JI, Jung SE, Kim PN, et al. Quality assurance in ultrasound screening for hepatocellular carcinoma using a standardized phantom and standard clinical images: a 3-year national investigation in Korea. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine 2014;33:985-95.
4. Marks RM, Ryan A, Heba ER, et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic Acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR Am J Roentgenol 2015;204:527-35.
5. Chou R, Cuevas C, Fu R, et al. Imaging Techniques for the Diagnosis of Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. Annals of internal medicine 2015;162:697-711.
6. Lee YJ, Lee JM, Lee JS, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology 2015;275:97-109.
7. Andersson KL, Salomon JA, Goldie SJ, Chung RT. Cost effectiveness of alternative surveillance strategies for hepatocellular carcinoma in patients with cirrhosis. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association 2008;6:1418-24.
Figures