0185
Traffic-Related Air Pollution Associated with Reduced Cortical Thickness and Altered White Matter Organization in a Longitudinally Studied, Pediatric Cohort1Radiology/Imaging Research Center, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 2Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 3University of Cincinnati College of Medicine, Cincinnati, OH, United States
Synopsis
Traffic-related air pollution (TRAP) is strongly associated with adverse cardiopulmonary health effects. Evidence suggests the developing brain may also be a target organ for particulate matter due to translocation either from the respiratory system or through the olfactory nerve. Using a pediatric cohort, we tested the hypothesis that exposure to TRAP during critical windows of brain development is significantly associated with changes in brain structure and organization. Children with high exposure levels at time of birth were associated with reductions in brain volume, cortical thickness, and diffusion abnormalities in white matter at 12 years compared with children at low exposure.
Purpose
Traffic-related air pollution (TRAP), a complex mixture of particulate matter (PM), metals, elemental and organic carbon, polycyclic aromatic hydrocarbons (PAH), and other constituents, is strongly associated with cardiopulmonary health effects [1]. Evidence suggests the developing brain may also be a target organ for these particles due to translocation either from the respiratory system or through the olfactory nerve [2]. Using an established pediatric epidemiological cohort with extensive longitudinal exposure assessment since infancy, we tested the hypothesis that exposure to TRAP during critical windows of brain development is significantly associated with changes in brain structure and organization. Our imaging study design targeted recruitment of participants from the cohort with the highest and lowest quartiles of exposure at time of birth.Methods
One hundred forty six participants (mean age 12.1 + 0.7 years, 57% male, 73% white, 55% high TRAP exposure) from the Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS) completed a high-resolution (1 mm3) anatomical imaging protocol with a 32-channel head coil at 3 Tesla. We evaluated brain volume and cortical thickness using the Computational Anatomy Toolbox for SPM 12 software running in Matlab. We derived diffusion metrics (fractional anisotropy (FA), mean (MD), axial (AD) and radial (RD) diffusivity) by employing a 32-direction, diffusion tensor imaging sequence (b values 0, 800 s/mm2). Analyses were performed using DTI Studio and custom software. Exposure to TRAP at birth was estimated using a previously developed land use regression model [3]. One-way ANOVA and multiple linear regression analyses were used to investigate the relationship between brain volume, cortical thickness, and diffusion metrics with TRAP exposure, respectively. Potential confounders and covariates were included in the analytical models.Results
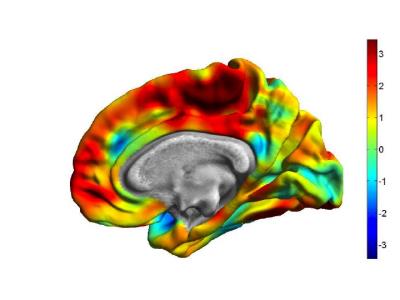
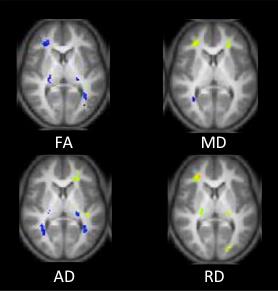
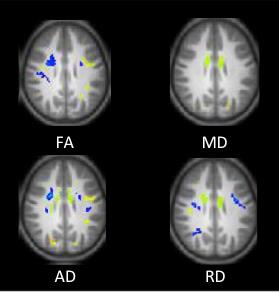
Children with high TRAP exposure levels at time of birth were associated with regionally specific reductions in brain volume, and cortical thickness, particularly within the posterior frontal lobe, at 12 years of age compared with children with low TRAP exposure (Figure 1). Higher exposed participants at birth demonstrated regions with diminished FA, increased MD, and RD within the right frontal lobe (Figure 2). In addition, higher exposed participants showed within the posterior left frontal lobe increased FA, AD and decreased RD (Figure 3).Conclusions
Children with higher exposure to TRAP demonstrate differences in brain structure and organization compared with their lower exposed peers. Different regional patterns may reflect variability in TRAP effects at time birth on the development of the brain cortex and white matter, especially with axonal structure and myelination.Acknowledgements
Funding for this project came from the National Institutes of Environmental Health Sciences (NIEHS) R01 ES019890.References
[1] Dockery DW, Ann Epidemiol 2009, 19:257-263
[2] Elder A, et al. Environ Health Perspect 2006, 114:1172-8
[3] Ryan PH, et al. Sci Total Environ 2008, 404:139-147
Figures