0149
One-sided hypoperfusion is associated with contralateral attention deficits in asymptomatic high-grade carotid stenosis patients.1Department of Neuroradiology, Technische Universität München, Munich, Germany, 2Philips Healthcare, Hamburg, Germany, 3Philips Healthcare, Best, Netherlands, 4Neuro-cognitive Psychology Unit, Department Psychologie, Ludwig-Maximillians-Universität, Munich, Germany
Synopsis
Patients with clinically asymptomatic, high-grade internal carotid artery stenosis (ICAS) often show cognitive impairments, such as memory dysfunction and attention deficits. However, it is still unclear whether these symptoms are caused by potentially reversible cerebral hypoperfusion or rather by a general unchangeable vascular damage. Here, 17 patients with one-sided high-grade, asymptomatic ICAS and 26 age-matched healthy controls underwent an MRI scan, including pCASL to assess brain perfusion, and a computer-based visual attention test. Patients show distinct unilateral cerebral hypoperfusion being significantly associated with contralateral attention deficits. Data indicate that chronic cerebral hypoperfusion in high-grade ICAS impairs cognitive function.
Purpose:
Patients with high-grade internal carotid artery stenosis (ICAS) often suffer from cognitive deficits, such as executive dysfunction, episodic memory impairment and attention deficits, even if they are clinically asymptomatic, i.e. do not show any signs of transient or permanent ischemic stroke symptoms 1-3. At the same time, some patients with unilateral ICAS also show perfusion reductions in the hemisphere ipsilateral to the stenosis, which are reversible by endovascular stenting or surgical endarterectomy 4. To date, it is unclear whether cognitive deficits are related to a global vascular damage or chronic hypoperfusion in patients with high-grade ICAS. In this still ongoing study, we assess the specific relation between one-sided cerebral blood flow (CBF) reductions and lateralized attention deficits.Methods:
17 patients (70.5±6.8, 5 female) with one-sided (right: n=12, left: n=5), high-grade, clinically asymptomatic ICAS (> 70%, according to the NASCET criteria) and 26 healthy, age-matched controls (70.7±4.8, 15 female) were enrolled in this prospective study. Participants underwent an MRI examination on a clinical 3T Ingenia scanner (Philips, Netherlands). The protocol included structural MRI (MP-RAGE and FLAIR sequences) as well as perfusion MRI using pCASL according to the recommendations of the ISMRM perfusion study group (3D readout, labeling planned based on PCA-survey, label duration 1800ms, post-label delay 2000ms, background suppression, voxel size: 2.73 x 2.86 x 6 mm3, 16 slices, 2 dynamics; Fig. 1) 5. CBF-maps were normalized to MNI space and mean CBF was extracted within each hemisphere’s watershed regions (CBF_right and CBF_left). An asymmetry index (AI) was calculated by the following formula: AI = (CBF_right) / (CBF_right + CBF_left). Furthermore, participants underwent a computer-based cognition test according to the theory of visual attention of Bundesen, which is a mathematically formulated model of selective attention 6. In brief, during this examination several letters are simultaneously displayed on the left and/or right visual hemifield. Participants are supposed to report as many letters as they could identify immediately after each run. By this method, critical global parameters of visual attention (processing speed C, visual short-term storage capacity K, and minimal effective presentation time t0) can be calculated. Furthermore, the spatial laterality of visual attention wλ can be estimated by a computational fitting of attentional weights (w) of the letters on each side which is calculated by the formula: wλ = (w_left) / (w_left + w_right). For group comparisons, we used two-sided two-sample t-tests with a significance level of p<0.05.Results:
Patients showed significantly reduced processing speed C (p=0.002; Fig. 2) and visual short-term storage capacity K with a trend to significance (p=0.081; Fig. 2). The minimal effective presentation time was significantly increased compared to controls (p=0.021; Fig. 2). Furthermore, there was a trend to significance of increased absolute spatial laterality of visual attention (|0.5-wλ|) in patients (p=0.088; Fig. 3). Concerning cerebral perfusion, patients showed a significantly higher absolute asymmetry (|0.5-AI|) than controls (p=0.001; Fig. 3). Most interestingly, AI correlated significantly with wλ in patients (r=0.538, p=0.039, Fig. 4) whereas no significant association was observed in controls (r=-0.122, p=0.554, Fig. 4).Discussion:
We revealed reduced global values of visual attention (C, K, and t0) in patients with clinically asymptomatic, high-grade ICAS. Patients also showed increased lateralization of attention deficits and cerebral perfusion. Perfusion asymmetry AI and spatial laterality of visual attention wλ correlated with each other in patients, i.e. unilateral hypoperfusion was associated with a contralateral visual attention deficit. PCASL, therefore, might offer a valuable, non-invasive technique to identify subjects with high-grade ICAS showing cerebral perfusion deficits being related to impaired brain function of the affected hemisphere, i.e. contralateral cognitive deficits.Conclusion:
These results indicate that cerebral hypoperfusion due to ICAS - as a potentially reversible state - impairs ipsilateral brain function, independently from a general vascular impairment. Whether both cerebral perfusion and cognitive function recover after endovascular or surgical treatment of ICAS needs to be elucidated in future studies.Acknowledgements
No acknowledgement found.References
1. Everts R, Wapp M, Burren Y, et al. Cognitive and emotional effects of carotid stenosis. Swiss medical weekly 2014;144:w13970.
2. Landgraff NC, Whitney SL, Rubinstein EN, et al. Cognitive and physical performance in patients with asymptomatic carotid artery disease. Journal of neurology 2010;257:982-91.
3. Mathiesen EB, Waterloo K, Joakimsen O, et al. Reduced neuropsychological test performance in asymptomatic carotid stenosis: The Tromso Study. Neurology 2004;62:695-701.
4. Kawai N, Hatakeyama T, Okauchi M, et al. Cerebral blood flow and oxygen metabolism measurements using positron emission tomography on the first day after carotid artery stenting. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 2014;23:e55-64.
5. Alsop DC, Detre JA, Golay X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine 2015;73:102-16.
6. Bundesen C. A theory of visual attention. Psychological review 1990;97:523-47.
Figures
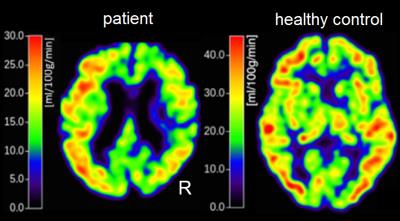
Fig. 1. Example of CBF maps.
Left: Patient with right-sided ICAS showing reduced CBF on the same side. Right: Healthy control with symmetrical cerebral perfusion.
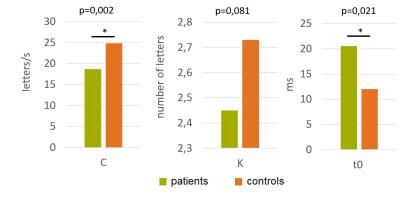
Fig. 2. Group differences of global visual attention parameters.
Bar plots of mean processing speed C, visual short-term storage capacity K and minimal effective presentation time t0 for patients (green) and healthy controls (orange). Patients showed significantly reduced C (mean patients: 18.7, controls: 24.8; two-sample t-test: p=0.002) and significantly increased t0 (mean patients: 20.6ms, t0 controls: 12.0ms; p=0.021). K was reduced in patients with a trend to significance (mean patients: 2.45, controls: 2.75; p=0.081).
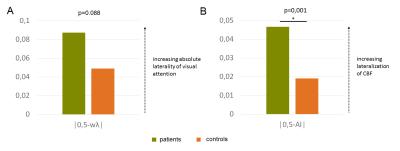
Fig. 3. Increased absolute laterality of spatial visual attention and cerebral perfusion in patients.
Bar plots of mean absolute spatial laterality of visual attention (|0.5-wλ|) and absolute lateralization of cerebral perfusion (|0.5-AI|) in patients (green) and healthy controls (orange). Patients showed increased one-sided attentional deficits with a trend to significance (mean patients: 0.087, mean controls: 0.049; two-sample t-test: p=0.088) and higher asymmetry of cerebral perfusion (mean patients: 0.047, mean controls: 0.019; p=0.001).
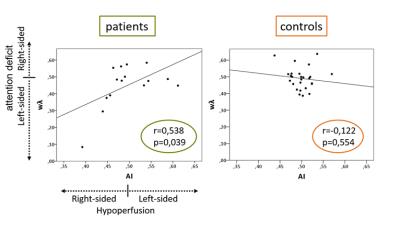
Fig. 4. Association of unilateral cerebral hypoperfusion and contralateral attentional deficits in patients.
Scatter plot and regression lines of each participant’s asymmetry index (AI) of cerebral perfusion and spatial laterality of visual attention (wλ) for patients (left) and healthy controls (right). Values above 0.5 of AI and wλ indicate hypoperfusion on the left side and attention deficits on the right side, respectively. On the contrary, values below 0.5 represent right-sided hypo-perfusion and left-sided attention deficits, respectively. Only patients showed a significant positive correlation of AI and wλ (r=0.538, p=0.039).