0141
An open-source hardware and software system for video-gated MRI1University of Applied Sciences and Arts Dortmund, Dortmund, Germany, 2Erwin L. Hahn Institute for Magnetic Resonance Imaging, University Duisburg-Essen, Essen, Germany, 3Division of Medical Physics in Radiology, German Cancer Research Center, Heidelberg, Germany
Synopsis
The limitations of contact-based hardware (e.g. electrocardiography, pulse oximetry) for cardiac activity measurement pose an obstacle in many ultra-high-field MRI examinations. In this work, we present a freely available hardware and software system for acquisition and processing of video signals from human skin that we developed with the aim to make this contact-free method available to other researchers.
Introduction
In ultra-high-field MRI, electrocardiography suffers from limitations that pose a major obstacle in daily practice1 and using pulse oximetry (PO) is problematic during long scans because patients frequently suffer from decreasing perfusion of the hands. We are interested in ultra-high-field non-enhanced angiography (MRA) of the lower extremities2, where an examination takes up to one hour and no adequate vendor-provided gating method is available due to the above-stated limitations.
Recently, video-based methods for the acquisition of a waveform similar to the one measured by PO have been presented3 that eventually might be used as an unobtrusive MRI gating method. In the context of MRI, methods for the acquisition of this waveform have been presented4-5 and cardiac gating has been proposed as future work4,6, but MR image acquisition has not yet been published, presumably due to the poor signal-to-noise ratio (SNR) of the video signal which is still inferior to PO.
In this work, we present a freely available (https://github.com/nspi/vbcg) hardware and software system for video-gated MRI that we developed with the aim to make this method available to other researchers and to enable practical usage by increasing SNR.
Methods
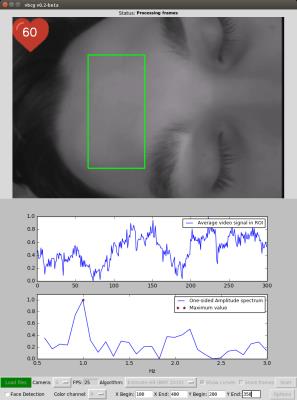
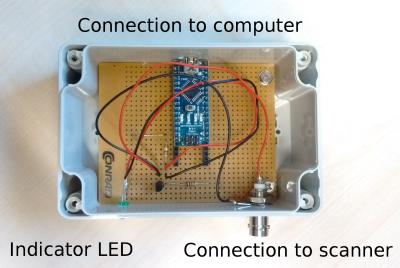
Video and trigger processing – The software contains algorithms for processing of videos from human skin in the context of MRI5-6. It is written in Python, published under an open-source license, and provides real-time feasibility as well as an interactive graphical user interface that is depicted in Fig. 1. Videos can be read from disk or live camera feed, a region-of-interest (ROI) can be defined, and results are visualized during runtime. Additionally, we developed a low-cost device for forwarding triggers to the MR scanner depicted in Fig. 2.
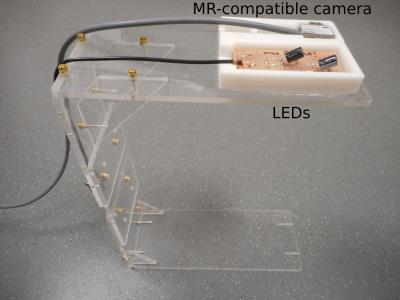
Video acquisition – As can be seen in Fig. 1 (upper plot), without applying additional measures, the SNR of the video signal is poor. Therefore, we built a camera stand, shown in Fig. 3, which supports ten LEDs (L-7113VGC-E, Kingbright, CA, USA; peak wavelength 518nm) next to the MR-compatible camera (12M-i, MRC Systems, Heidelberg, Germany; integrated LED, peak wavelength 950nm).
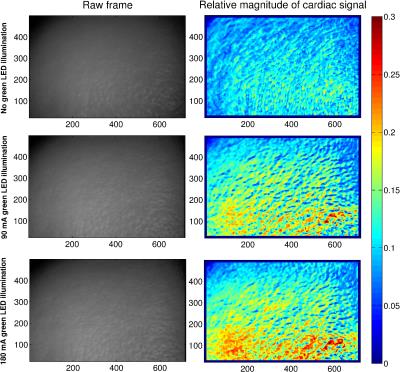
Experiment – An experiment was conducted to quantify the effect of illumination on the SNR and in turn on gating accuracy. A volunteer lay on the patient table in a 7T MR room (Magnetom, Siemens GmbH, Erlangen, Germany) with the stand oriented so that the camera was aimed toward his forehead. Room lighting was turned off to avoid bias. Video data (30Hz sampling rate) and MR vendor-provided PO (50Hz) as ground truth were stored in three 60s stages: 1) dedicated LED illumination turned off, 2) set to 90mA, and 3) set to 180mA. Values above 180mA caused pixel saturation. The camera-integrated infrared LED was used during all stages.
Results
Fig. 4 shows maps that depict the spatial distribution of the cardiac signal magnitude. As can be seen, by increasing LED illumination, the SNR of the signal, i.e. the relative magnitude of heart rate frequencies to other frequencies, increases as well and reaches a maximum of approx. 30% for 180mA illumination. Note the absence of contiguous areas on the skin surface with high SNR, rather scattered regions with variably higher and lower values dominate.
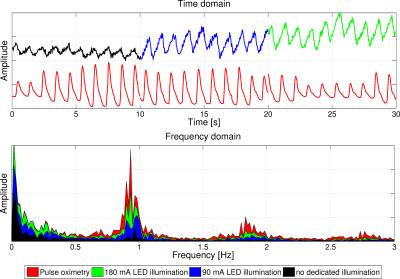
Fig. 5 compares the PO signal to the video signal and shows that they become more similar with increasing illumination. Using the proposed software, we applied a cardiac gating algorithm5 (N=300, mov. avg.=100) on the videos with a ROI covering the entire area of the frames. The computed triggers had a mean trigger-to-trigger duration of 1050.6ms (no illumination), 1080.6ms (90mA), and 1103.5ms (180mA) and standard deviation of 205.9ms, 157.9ms, and 107.2ms, respectively. Compared to PO triggers, computed by the MR vendor-provided software, this results in a difference in means of 30.4ms, 18.8ms, and 5.0ms and difference in standard deviation of 53.3ms, 95.6ms, and 43.2ms, respectively.
Discussion and Conclusion
This work underlines the importance of illumination when acquiring video signals of the human skin for estimating the cardiac activity. The results show that increasing illumination improves the SNR of the cardiac signal and in turn improves gating accuracy, measured by comparing our trigger-to-trigger durations with PO trigger-to-trigger durations.
The limitations of contact-based gating methods pose an obstacle in many ultra-high-field examinations, e.g. MRA. Using unobtrusive video-based methods could overcome some of these limitations. The development of the proposed system was motivated to make this field of research accessible to other researchers. It is published (https://github.com/nspi/vbcg) on a widely-used, collaboration-oriented hosting service and we encourage to use and modify the source code and hardware specifications.
Acknowledgements
No acknowledgement found.References
1. Snyder CJ, DelaBarre L, Metzger GJ, et al. Initial results of cardiac imaging at 7 tesla. Magnetic Resonance in Medicine 2009;61(3):517-524
2. Fischer A, Maderwald S, Orzada S, et al. Nonenhanced Magnetic Resonance Angiography of the Lower Extremity Vessels at 7 Tesla. Investigative Radiology 2013;48(7):525-534
3. Sun Y, Thakor N. Photoplethysmography Revisited: From Contact to Noncontact, From Point to Imaging. IEEE Transactions on Biomedical Engineering 2015;63(3):463-477
4. Maclaren J, Aksoy M, Bammer R. Contact-free physiological monitoring using a markerless optical system. Magnetic Resonance in Medicine 2015;74(2):571-577
5. Spicher N, Maderwald S, Ladd ME, et al. Heart rate monitoring in ultra-high-field MRI using frequency information obtained from video signals of the human skin compared to electrocardiography and pulse oximetry. Current Directions in Biomedical Engineering 2015;1(1):69-72
6. Spicher N, Kukuk M, Ladd ME, et al. In vivo 7T MR imaging triggered by phase information obtained from video signals of the human skin. Proceedings ISMRM 2015 (#2548)
Figures