0123
Liver Fat Reduction Following Bariatric Weight Loss Surgery is Greater in the Right Lobe of the Liver1Liver Imaging Group, Department of Radiology, University of California San Diego, San Diego, CA, United States, 2Computational and Applied Statistics Laboratory, University of California San Diego, San Diego, CA, United States, 3Department of Radiology, Medical Physics, Biomedical Engineering, Medicine, and Emergency Medicine, University of Wisconsin Madison, Madison, WI, United States
Synopsis
As liver fat is heterogeneously distributed, longitudinal changes in liver fat may vary between liver segments. We used confounder-corrected chemical-shift-encoded MRI to examine longitudinal changes in proton density fat fraction (PDFF) of individual liver segments in obese adults following a weight-loss program comprising a very low calorie diet (VLCD) followed by bariatric weight loss surgery (WLS). We observed that changes in PDFF in the 5-month postoperative period vary across segments, with right-lobe segments having more rapid reduction in liver fat.
Introduction
Proton density fat fraction (PDFF) is a standardized MR biomarker of liver fat content 1,2 and can be used for non-invasive monitoring of liver fat longitudinally 3. As liver fat is heterogeneously distributed 4, longitudinal changes in liver fat may vary between liver segments. The purpose of this study was to examine longitudinal changes in PDFF of individual liver segments during a weight-loss program comprising 2-4 weeks of very low calorie diet (VLCD) followed by bariatric weight loss surgery (WLS).Methods
We performed a secondary analysis of prospectively collected data in initially morbidly obese adult patients who participated in a VLCD-WLS weight loss program. Patients were recruited consecutively from two bariatric surgery centers over 66 months. Demographic data was collected and summarized descriptively. PDFF was estimated using confounder-corrected chemical-shift-encoded MRI (CSE-MRI) 1 in each hepatic segment at baseline (visit 1), immediately after completion of VLCD (visit 2), and at 1, 3, and 6 months (visits 3-5) after WLS. A linear regression model with a random (subject-specific) intercept was used to estimate the slope of time-dependent PDFF decline separately for visit 1-2 data and for visit 3-5 data for each hepatic segment. The slopes for all segments were then compared pairwise for each time period using bootstrap-based tests with Bonferroni adjustment for multiple comparisons.Results
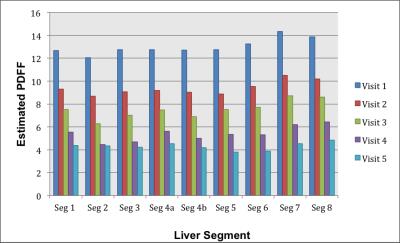
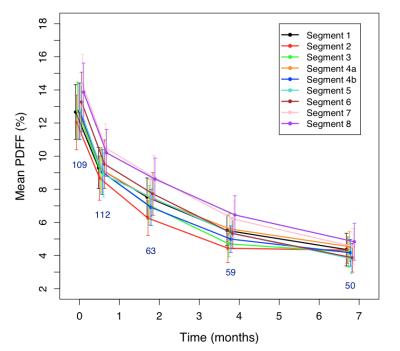
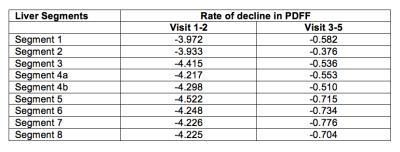
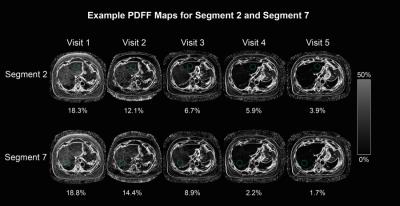
123 patients were enrolled (102 female, 21 male; mean age of 48.0 ± 13.0). Figure 1 shows the mean PDFF, by liver segment, and by visit number. Segment 7 had the highest PDFF and segment 2 the lowest PDFF at baseline. Figure 2 shows longitudinal decline in estimated PDFF by liver segment. For all segments, the rate of decline for visit 1-2 was significantly greater than the rate of decline for visit 3-5 (Table 1). For visits 1-2, there were no statistically significant pairwise differences in slope between segments after Bonferroni correction. For visit 3-5, several pairwise differences were statistically significant (5, 6 and 8 vs. 2; 7 vs. 3, 4a and 4b; 8 vs. 4b): in each case, a right-lobe segment had greater decline than a left-lobe segment. Segment 7 had the highest and segment 2 had the lowest rate of decline. An example of series of PDFF maps for segment 2 and segment 7 in an individual patient is shown in Figure 3.Discussion
Our study is the first to describe longitudinal changes in PDFF by liver segments during a VLCD-WLS weight loss program. We observed that longitudinal changes in PDFF during the preoperative 2-4 week VLCD were similar between segments. However, changes in the 5-month postoperative period varied across segments, with right-lobe segments having more rapid reduction in liver fat content. Heterogeneity in liver fat distribution has been previously described in cross-sectional studies 4. Our findings show that changes in liver fat content following WLS is also non-uniform. Thus, methods that do not provide whole-liver fat assessment, such as liver biopsy, may be unreliable in monitoring longitudinal changes in liver fat. By estimating a composite PDFF from all nine Couinaud segments, CSE-MRI may be more reliable than liver histology for this purpose.Conclusion
We found small but statistically significant differences in longitudinal changes of fat content following WLS among liver segments. Overall, segments in the right lobe had more rapid decline in fat content than segments in the left lobe. Segments with greater baseline fat content had larger declines in fat content following WLS.Acknowledgements
We acknowledge NIH R01 DK083380, R01 DK088925, R01 DK100651, and K24 DK102595 grants, and GE Healthcare for providing support to the University of Wisconsin and University of California at San Diego.References
1. Reeder SB, Hu HH, Sirlin CB. Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration. J Magn Reson Imaging 2012;36:1011-1014.
2. Meisamy S, Hines CD, Hamilton G, Sirlin CB, McKenzie CA, Yu H, et al. Quantification of hepatic steatosis with T1-independent, T2-corrected MR imaging with spectral modeling of fat: blinded comparison with MR spectroscopy. Radiology 2011;258:767-775.
3. Le TA, Chen J, Changchien C, Peterson MR, Kono Y, Patton H, et al. Effect of colesevelam on liver fat quantified by magnetic resonance in nonalcoholic steatohepatitis: a randomized controlled trial. Hepatology. 2012;56(3):922-32.
4. Bonekamp S, Tang A, Mashhood A, Wolfson T, Changchien C, Middleton MS, et al. Spatial distribution of MRI-Determined hepatic proton density fat fraction in adults with nonalcoholic fatty liver disease. J Magn Reson Imaging. 2014;39(6):1525-32.
Figures