0098
The prognostic power of early and late phase DCE-MRI parameters in locally advanced cervix cancer.1Dept og Radiology and Nuclear Medicine, Oslo University Hospital, Oslo, Norway, 2Dept. of Radiation Biology, Institute of cancer Research, Oslo University Hospital, Oslo, Norway, 3Dept. of Gynecological Cancer, Oslo University Hospital, Oslo, Norway, 4Institute for Cancer Genetics and Informatics, Oslo University Hospital, Oslo, Norway, 5Institute for Clinical Medicine, University of Oslo, Oslo, Norway
Synopsis
DCE-MRI can provide prognostic information on locally advanced cervix carcinomas. Most studies have emphasis on the early phase of the Signal Intensity Time Curve (SITC). The purpose of this study was to explore the prognostic value of the late phase of the SITC and to reveal any added value to that of parameters from the early phase. Both the early phase parameter LETV and the late phase parameter TVIS was associated with overall survival. The association was independent of clinical factors like tumor volume, FIGO stage and lymph node status. TVIS did not provide any added prognostic value to LETV.
Introduction
Hypoxia is a known adverse prognostic factor in locally advanced cervix carcinomas showing association with treatment failure and poor survival. Evidence from clinical and preclinical investigations confirms that dynamic contrast-enhanced magnetic resonance imaging (DCE- MRI) with Gd-DTPA can provide information on the oxygenation of cervix carcinomas (1-3). Various parameters from both semi-quantitative and quantitative analysis of DCE-MRI are shown to be predictive of relapse and mortality (4-8), though none are yet a part of routine clinical imaging. In this study we looked at the Signal Intensity versus Time Curves (SITC) with a voxel-by-voxel approach aiming to characterize traits in the SITC reflective of hypoxia. As most studies have focused on the early part of the SITC, we wanted to explore whether the late-phase SITC could provide additional and more powerful DCE-MRI-based prognostic parameters. In the early phase of the SITC, poor enhancement is thought to reflect poor perfusion and hypoxia. For the late phase an ascending SITC in a voxel implies slow diffusion of contrast agent into the voxel. Voxels showing ascending late-phase SITCs are therefor most likely localized in poorly vascularized tumor regions characterized by hypoxia and/ or necrosis. By using a simple semi-quantitative approach, we focused on both the early and the late phase SITC, comparing the two.Method
Eighty-five patients with locally advanced cervical cancer admitted to our institution between 2004 and 2007 were included in our study. All were treated with cisplatin-based concurrent chemo-radiotherapy with a curative intent. Briefly pretreatment DCE-MRI was carried out using an axial T1-weighted spoiled gradient sequence (TR=160ms, TE=3.5ms, α=900, field of view: 20x20cm2, image matrix: 256x 256, number of excitations: 1, slice thickness: 5mm, slice spacing: 6mm, scan time >9minutes post-contrast). Tumors were delineated by examining DCE-MRI and T2-weighted images in the open source dicom viewer Osirix. Due to poor signal-to noise ratios, 5 of the 85 patients were excluded from the late-phase analysis. Endpoints were time from diagnosis to relapse or death censored at end of follow-up.
For every voxel the SITC was calculated. Early phase was defined as the first 60 seconds and late phase as the interval between 3 and 9 minutes after IV administration of contrast. Early phase Low-Enhancing Tumor Volume (LETV) was calculated as previously described (9). For the late phase we calculated a Tumor Volume of Increasing Signal (TVIS), adding up all voxels were the SITC showed a continuous rise (fig1). The population was dichotomized into low/middle and upper tertile according to LETV/TVIS as described earlier (9). Endpoints were compared using the log rank test, the results presented as Kaplan-Meier plots. Multivariate cox regression analysis including the DCE MRI- and clinical parameters was performed to identify prognostic factors of survival.
Results
In the early phase of the SITC, tumors with a high LETV did significantly worse than the ones with a low/middle LETV. In the late phase, tumors with a high TVIS did significantly worse than those with a low/middle TVIS. The results applied for both Overall and Disease-free Survival (fig2). In multivariate analysis including the clinical parameters tumor volume, lymph node status and FIGO stage, both LETV and TVIS were independent prognostic factors of Disease-free and Overall Survival. When adding both DCE-MRI parameters in a multivariate analysis, the independent prognostic power of either parameter was lost (table1).
Discussion
DCE-MRI provides prognostic information in addition to clinical factors and this information is available even when using simple semi-quantitative methods without advanced pharmacokinetic modelling. Both our early and late phase parameters are thought to reflect on tumor hypoxia and both showed prognostic value for the outcome of locally advanced cervical cancer. Both parameters have advantages and disadvantages. TVIS requires a long scan time while LETV only needs a DCE-MRI of 1-2minutes. The calculation of LETV is dependent on defining a threshold in signal intensity to separate low-enhancing from high-enhancing voxels. This threshold is sensitive to MRI scanner and protocol, making validation a challenge. The TVIS is calculated from the slope of the SITC and less sensitive to scanning parameters, making it easier to compare across institutionsConclusion
Both the early phase parameter LETV and the late phase parameter TVIS was associated with survival. As the late phase parameter did not provide any additional prognostic power when compared to the early phase it is hard to justify the long scan time needed to obtain them.Acknowledgements
Thanks to the staff at the Dept. of Radiology, the Norwegian Radium Hospital, especially Kjetil Knutstad MD and Hans Henrik Lien MD PhD for their support, professional and academic, in contribution to this study.References
1. Ellingsen C, Hompland T, Galappathi K, Mathiesen B, Rofstad EK. DCE-MRI of the hypoxic fraction, radioresponsiveness, and metastatic propensity of cervical carcinoma xenografts. Radiother Oncol. Elsevier Ireland Ltd; 2014 Feb 1;110(2):335–41.
2. Lyng H, Vorren AO, Sundf r K, Taksdal I, Lien HH, Kaalhus O, et al. Assessment of tumor oxygenation in human cervical carcinoma by use of dynamic Gd-DTPA-enhanced MR imaging. J Magn Reson Imaging. 2001;14(6):750–6.
3. Cooper RA, Haider MA, Loncaster JA, Todd SM, Yeung I, Logue JP, et al. Tumour oxygenation levels correlate with dynamic contrast-enhanced magnetic resonance imaging parameters in carcinoma of the cervix. Radiother Oncol. 2000 Oct 1;57(1):53–9.
4. Zahra MA, Hollingsworth KG, Sala E, Lomas DJ, Tan LT. Dynamic contrast-enhanced MRI as a predictor of tumour response to radiotherapy. The Lancet Oncology. 2007 Jan;8(1):63–74.
5. Yuh WTC, Mayr NA, Jarjoura D, Wu D, Grecula JC, Lo SS, et al. Predicting Control of Primary Tumor and Survival by DCE MRI During Early Therapy in Cervical Cancer. Investigative Radiology. 2009 Jun;44(6):343–50.
6. Yamashita Y, Baba T, Baba Y, Nishimura R, Ikeda S, Takahashi M, et al. Dynamic contrast-enhanced MR imaging of uterine cervical cancer: Pharmacokinetic analysis with histopathologic correlation and its importance in predicting the outcome of radiation therapy. Radiology. 2000;216(3):803–9.
7. Mannelli L, Patterson AJ, Zahra M, Priest AN, Graves MJ, Lomas DJ, et al. Evaluation of Nonenhancing Tumor Fraction Assessed by Dynamic Contrast-Enhanced MRI Subtraction as a Predictor of Decrease in Tumor Volume in Response to Chemoradiotherapy in Advanced Cervical Cancer. American Journal of Roentgenology. 2010 Aug;195(2):524–7.
8. Hawighorst H, Weikel W, Knapstein PG, Knopp MV, Zuna I, Schönberg SO, et al. Angiogenic activity of cervical carcinoma: assessment by functional magnetic resonance imaging-based parameters and a histomorphological approach in correlation with disease outcome. Clin Cancer Res. 1998 Oct 1;4(10):2305–12.
9. Lund KV, Simonsen TG, Hompland T, Kristensen GB, Rofstad EK. Short-term pretreatment DCE-MRI in prediction of outcome in locally advanced cervical cancer. Radiotherapy and Oncology. 2015 Jun;115(3):379–85.
Figures
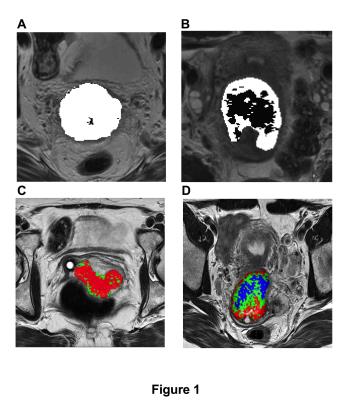
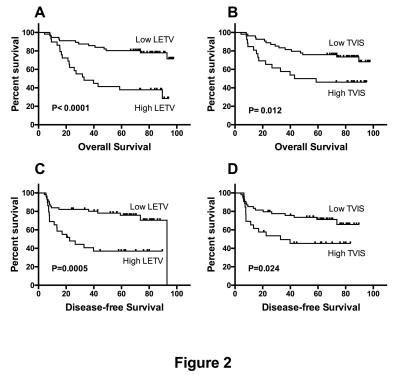
Figure 2
Kaplan-Meier curves for Overall Survival and Disease-free Survival stratified by the early phase parameter LETV (A and C) and the late phase parameter TVIS (B and D) showing significant lower survival in patients with a high LETV or TVIS compared to patients with a low LETV or TVIS
