Jill M Slade1, Anne Tonson2, David Hurley1, Mitchell Rozman1, George S Abela3, and Ronald A. Meyer2
1Radiology, Michigan State University, East Lansing, MI, United States, 2Physiology, Michigan State University, 3Medicine, Michigan State University
Synopsis
Functional MRI (BOLD) of skeletal muscle was used to
evaluate changes in microvascular function before and after aerobic exercise
training in older adults. Peak BOLD responses increased by ~30% after exercise
training, supporting the use and sensitivity of BOLD MRI to assess changes in microvascular
function.
Introduction
Peripheral microvascular function is clearly
reduced with age (1,2,8) even when comparing sedentary young and older adults
(1). This is important because declines in microvascular function may
contribute to reduced muscle performance and activity limitations in
aging. Furthermore, the microvasculature
has been shown to be crucial in the control of blood flow (3) and microvascular
dysfunction has been implicated in many chronic diseases (4,5). Blood Oxygen
Level Dependent (BOLD) imaging of skeletal muscle using functional magnetic
resonance imaging (fMRI) can be used to assess microvasculature function (2,6,7).
Microvascular function is greater in healthy endurance trained young adults
compared to sedentary young adults (8). This suggests that exercise training
may be used to enhance small vessel function. The study aimed to assess changes
in microvascular function using BOLD MRI in older adults following aerobic
exercise training.Methods
Twenty five healthy,
sedentary older adults participated in a 12-week randomized graded treadmill
walking intervention (control (CON), n=13, 66±4 yrs, BMI=31±6; exercise (EX),
n=16, 68±6 yrs, BMI=29±5; mean±SD). Walking was done 4 days a week for 45
minutes at 70% heart rate reserve. Controls were asked to maintain a sedentary
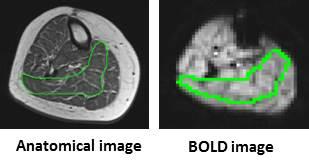
lifestyle. GE Excite 3T MRI and a quadrature extremity coil were used to
acquire images of the calf. T2* weighted images were used to acquire
microvascular BOLD images using a gradient recalled echo planar sequence (TR/TE=1000/35
ms, 60 degree pulse, 1cm slice, 64x64 matrix). Maximal voluntary plantar
flexion contractions (1 s in duration) were performed once every 90 s for a
total of five contractions to examine contraction induced peak BOLD. Anatomical
images of the entire leg were also acquired (TR/TE=600/12.4ms, 256x192 matrix).
31P MR spectroscopy was used to quantify oxidative capacity of the
plantar flexor muscles before and after training. Spectra were acquired using a
12cm surface coil placed under the calf (51.7MHz, TR=3s. 2500Hz sweep, 60°
pulse). Subjects performed 30-s of plantar flexion at 0.7 Hz for a total of 20
contractions. BOLD responses of the soleus muscle were averaged over the highest 2-4
contractions with respect to BOLD response and force. MRS data were processed
with JMRUI AMARES algorithm. A monoexponential model was used to fit the time
constant of phosphocreatine recovery following exercise. Repeated measures ANOVA was used to assess
differences between groups with significance at p <0.05. Results and discussion
Peak post-contraction BOLD response
in the soleus increased by ~30% in EX (PRE= 103.5±1.4%, POST=104.5±1.6%)
compared to CON (PRE: 103.6±1.9%, POST: 103.6±1.7%); Fig. 2, a significant interaction
was present between time and group, p = 0.019. Muscle oxidative capacity (tau,s) of the
plantar flexors improved by 34% for EX compared to CON (Fig. 3); a significant
interaction was present over time between groups, p = 0.001. These findings show that age
related declines in small vessel function can be improved with moderately
intense exercise. BOLD MRI can be used
to evaluate changes in microvascular function. Acknowledgements
Supported by NIH AG042041References
(1) Slade JM, Noble K et al., Med Sci Sport Exerc
46(S5): S354, 2014. (2) Slade JM, Towse TF, et al., J Appl Physiol
111(5):1361-71, 2011. (3) VanTeeffelen JW, and Segal SS. Am J Physiol Heart
Circ Physiol 290: H119-127, 2006. (4)Robbins JL, Jones et al., J Appl Physiol
111(1):81-6, 2011. (5) Vithian K, and Hurel S. Clin Med 10:
505-509, 2010. (6) Meyer RA, Towse TF, et al., NMR Biomed 17:392–398,
2004. (7) Towse TF, Slade JM, et al., J Appl Physiol
111(1): 27-39, 2011. (8) Hughes WE, Ueda K, et al., Physiol Rep. 3(8):
e12516, 2015.