0055
Evaluation of Myelin Damage in Diffuse Traumatic Brain Injury using ViSTa-MWI1Department of Electrical and Computer Engineering, Seoul National University, Seoul, Korea, Republic of, 2CUNY School of Medicine, The City College of New York, New York, NY, United States, 3Moss Rehabilitation Research Institute, Elkins Park, PA, United States
Synopsis
This study investigated myelin damage in subacute moderate to severe TBI using ViSTa-MWI. The results showed widespread reductions of MWF in patients, consistent with pathology involving diffuse axonal injury. Furthermore, the extent of myelin damage was strongly correlated with measures of injury severity and cognitive impairment, demonstrating its clinical relevance.
Purpose
Traumatic brain injury (TBI) is one of the leading causes of death and permanent disability worldwide [1]. Traumatic axonal injury, or diffuse axonal injury, is a hallmark of TBI and more predictive of behavioral outcome than focal injury in case of moderate to severe TBI [2]. However, accurate assessment of the axonal damage is still challenging using conventional MR images (e.g. T1w and T2w images). Myelin, which is not distinguishable on T1w or T2w images, has increasingly been considered an important component in the pathophysiology of TBI. In animal studies, TBI mice have shown significant myelin loss from 3 days to 6 weeks post-TBI compared to sham surgery using electron microscopy [3]. More recently, a human in vivo study using myelin water imaging (MWI), which is a biomarker for myelin, has revealed a reduction in myelin water fraction (MWF) at 2 weeks post-injury in mild TBI patients [4]. However, few studies have focused on moderate to severe TBI patients to evaluate the pattern of white matter myelin injury. Furthermore, the conventional MWI used in the previous mild TBI studies, has limited image quality due to ill-conditioned data fitting process. In this study, we investigated the extent of myelin damage in moderate to severe in vivo human TBI patients using a new MWI method (ViSTa-MWI) that provides improved image quality. We compared TBI patients with healthy controls (HC) on MWF using voxel-wise TBSS analysis. Additionally, we evaluated the clinical relevance of MWF by assessing its correlations with overall injury severity and post-traumatic impairment in cognitive processing speed.Methods
Twenty three TBI patients at 3 months post-injury and 30 HC were scanned at 3T (IRB-approved). ViSTa-MWI: a 3D segmented EPI based ViSTa sequence [5] was implemented using the following parameters: resolution = 1.38x1.38x5 mm3, 26 slices, TR/TE=1160/4.5 ms, TI1/TI2/TD=560/220/380 ms, partial k-space=6/8, EPI factor=15, and scan time=7 min 33 sec. To quantify MWF, a PDw GRE sequence based on the same EPI as the ViSTa sequence was acquired (TR=97 ms, flip angles=6° for Figure 1 and 28° for data analysis, and each scan time=38 sec). The ViSTa-MWF was calculated by dividing the ViSTa data by the PDw GRE data and multiplying a scaling factor [5]. The resulting ViSTa-MWF is referred to as apparent MWF (aMWF) due to the scaling factor. Data processing and analysis: For TBSS analysis, all ViSTa-MWI images were first registered non-linearly to a JHU FA map using SyN in ANTs [6, 7]. A mean skeleton was then generated using the registered ViSTa-MWI images for subsequent group-level analysis. To examine group difference of aMWF between TBI and HC, a two-sample permutation t-test was performed by “randomise” in FSL [8] for each voxel on the skeleton. Age and gender were used as covariates of the statistical analysis and the family-wise error (FWE) rate corrected p-value was used. To compare the mean global aMWFs in TBI with those in HC, all voxels on the skeleton were averaged for each subject. Mann Whitney U test was used to evaluate statistical difference between TBI and HC in global aMWF (p<0.05). Additionally, to evaluate clinical relevance of MWF, Pearson’s correlation coefficients were calculated between global TBI aMWFs and the Processing Speed Index (PSI) from the WAIS-IV [9] and also between global TBI aMWFs and the duration of Post Traumatic Amnesia (PTA).Results
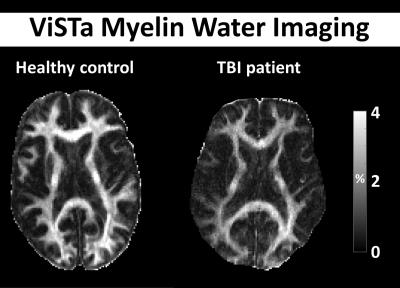
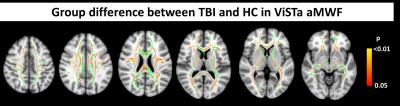
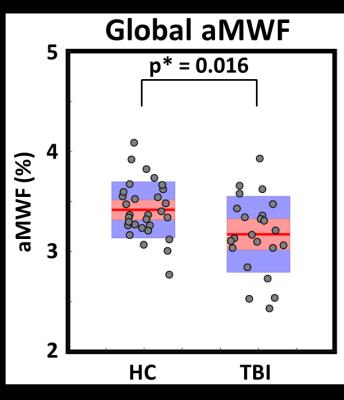
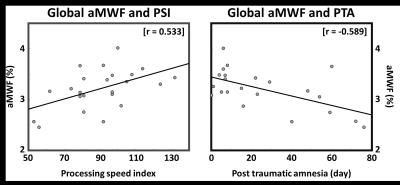
Figure 1 shows that aMWF values in TBI are smaller than those in HC in broad areas of the brain. A voxel-wise comparison of aMWF between the two groups shows statistically significant widespread reductions in TBI patients’ aMWFs compared to those in HC (p*<0.05, Fig. 2), demonstrating that diffuse injury causes spatially substantial damage to myelin. To support that, in comparison of mean global aMWFs, the aMWF values in TBI were reduced relative to HC (HC=3.4±0.3% and TBI=3.2±0.4%, percentage decrease=5.9%) (Fig. 3). Regarding the relationship between global TBI aMWF and PSI (r=0.533) and between global TBI aMWF and PTA (r=-0.589), significantly strong correlations were found (Fig. 4), suggesting myelin damage may be clinically relevant to diffuse TBI.Discussion and Conclusion
In this study, we demonstrate that reduced MWF, quantified by ViSTa-MWI, is prevalent in subacute, moderate to severe TBI with mostly diffuse pathology. A robust relationship of MWF with PTA and PSI suggests that myelin damage could serve as a potential biomarker for injury severity and post-traumatic clinical outcomes in diffuse TBI. Future studies should focus on the relationship between MWF and existing general DTI measures in this condition.Acknowledgements
This work was supported in part by the NIH grant 5R01NS065980, by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2015R1D1A1A01058360), and by the Brain Korea 21 Plus Project in 2016.
References
1. Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728-741.
2. Ross DT, Meaney DF, Sabol MK, et al. Distribution of forebrain diffuse axonal injury following inertial closed head injury in miniature swine. Exp Neurol. 1994;126(2):291-299.
3. Mierzwa AJ, Marion CM, Sullivan GM, et al. Components of myelin damage and repair in the progression of white matter pathology after mild traumatic brain injury. J Neuropathol Exp Neurol. 2015;74(3):218-232.
4. Wright AD, Jarrett M, Vavasour I, et al. Myelin Water Fraction Is Transiently Reduced after a Single Mild Traumatic Brain Injury--A Prospective Cohort Study in Collegiate Hockey Players. PLoS One. 2016;11(2):e0150215.
5. Oh SH, Bilello M, Schindler M, et al. Direct visualization of short transverse relaxation time component (ViSTa). Neuroimage. 2013;83:485-492.
6. Avants B, Gee JC. Geodesic estimation for large deformation anatomical shape averaging and interpolation. Neuroimage. 2004;23 Suppl 1:S139-150.
7. Avants BB, Yushkevich P, Pluta J, et al. The optimal template effect in hippocampus studies of diseased populations. Neuroimage, 2010;49(3):2457-2466.
8. Winkler AM, Ridgway GR, Webster MA, et al. Permutation inference for the general linear model. Neuroimage. 2014;92:381-397.
9. Wechasler D, Coalson D, Raiford S. WAIS-IV: Wechsler adult intelligence scale. San Antonoio, TX, Pearson, 2008.
Figures