James W Goldfarb1, Usama Hasan1, and Jie J Cao1
1St Francis Hospital, Roslyn, NY, United States
Synopsis
Myocardial fat
content, R2*/T2* and off-resonance frequency can be measured with high
resolution using a native MR water-fat separation imaging technique applied to
multiple gradient echo images. Significant differences in myocardial fat
fraction were found consistent with fatty metaplasia in a subset of chronic
myocardial infarction patients. Off-resonance and T2* changes consistent with
intramyocardial hemorrhage were observed in a subset of acute myocardial
infarction patients.
Introduction
Multiple gradient echo
imaging allows the joint quantification of myocardial T2*/R2*, off -resonance
frequency and fat fraction. In a single breath-hold, three native maps of
independent MR properties can be obtained for quantitative myocardial tissue
characterization. Fatty metaplasia has been shown in chronic myocardial
infarction and non-ischemic cardiomyopathies associated with diabetes and
obesity. Changes in T2* and off-resonance frequency due to susceptibility
changes have been associated with hemorrhagic myocardial infarction and
hemochromatosis. The goal of this study was to obtain normal ranges of the
three native parameters maps and investigate their use in acute and chronic
myocardial infarction (MI).Methods
48 subjects (17 normal
control, 11 Acute MI at 3 days and 20 Chronic MI >2 yrs) were studied at
1.5T with native joint R2*/T2*, off-resonance and fat fraction mapping using a
multipeak model with R2* and B0 corrections [1] in parallel short and long axis
slice views spanning the entire left ventricle.The water-fat separation
framework provides four images: water only, fat only, R2* and off-resonance.
Off resonance maps were high-pass filtered to remove B0 field contributions.
Additionally, conventional bSSFP CINE and late gadolinium-enhanced (LGE)
imaging (0.15 mmol/kg) were obtained. Mean parameter values were measured in
the heart (16 segment AHA model). Parameter maps were visually evaluated for
focal lesions. Normal segmental differences and associations with LGE presence
and age of MI were evaluated with statistical tests (ANOVA).Results
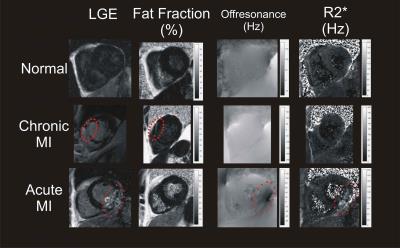
Focal fatty metaplasia
was visualized in a subset of chronic MI patients (n=12). T2* and off-resonance
segmental changes were also well visualized in a subset of acute MI patients
(n=3) (See Figure 1, red circles). Focal myocardial fat lesions had an
admixture of water and fat signal fat fraction = 52.8% ±14.6. Figure 2 shows
acute and chronic MI parameters compared with normal values. Fat fraction was
significantly higher in chronic myocardial infarction (16.7% ± 12.9 vs 2.8% ±
2.1, p < 0.001). Off-resonance frequency was significantly lower in both
chronic and acute myocardial infarction (3.2 Hz ±22.6 vs 20.9 Hz ± 21.6,
p=0.01). 18 chronic MI patients had fat fractions outside of the normal range
(18.4% ± 12.4 vs 2.8% ± 2.1, p < 0.001). Three acute MI patients had R2*
values and off-resonance frequencies outside of normal ranges and all
demonstrated MVO in LGE images consistent with intramyocardial hemorrhage.Discussion
Myocardial fat content, R2*/T2* and off-resonance frequency can be
measured with high resolution using a native MR water-fat separation imaging
technique applied to multiple gradient echo images. Significant differences in
myocardial fat fraction were found consistent with fatty metaplasia in a subset
of chronic MI patients. Off-resonance and T2* changes consistent with
intramyocardial hemorrhage were observed in a subset of acute MI patients.Acknowledgements
No acknowledgement found.References
1. Hernando D, Kellman
P, Haldar JP, Liang ZP. Robust water/fat separation in the presence of large
eld inhomogeneities using a graph cut algorithm. Magn Reson Med
2010;63(1):79-90.