0035
PET/MR Imaging of Metabolic Bone Activity in Osteoarthritis1Radiology, Stanford University, Stanford, CA, United States, 22Department of Mechanical Engineering, University of Saskatchewan, Saskatoon, SK, Canada, 3Department of Radiology & Nuclear Medicine, Erasmus MC, University Medical Center, Rotterdam, Netherlands, 4Department of Bioengineering, Stanford University, Stanford, CA, United States, 5Department of Orthopaedic Surgery, Stanford University, San Francisco, CA, United States
Synopsis
Osteoarthritis (OA) is a leading cause of disability, resulting in reduced quality of life, at tremendous societal cost. New hybrid PET/MR systems allow for simultaneous, sensitive, and quantitative assessments of early bone activity in OA with PET, which can be correlated with high-resolution quantitative MR methods of soft tissues to study the pathogenesis of OA. We demonstrate promising initial results of simultaneous PET/MR hybrid imaging of knee OA. Results suggest that PET/MR may detect metabolic abnormalities in subchondral bone, which appear normal on MRI. These advancements will allow us to detect and track early and reversible changes in OA.
Purpose
Osteoarthritis (OA) is a chronic, degenerative disease of the joint that affects 14 million Americans, causing joint pain, stiffness and loss of mobility1. OA is characterized by degeneration affecting all tissues in the joint. Magnetic resonance imaging(MRI) provides an excellent opportunity to non-invasively study and understand complex disease processes involved in OA2. However, characterization of bone pathology on MRI is limited to qualitative assessment of osteophytes and marrow signal changes3 and is poorly understood. 18F-fluoride is a long recognized bone-seeking PET radiotracer that is able to probe bony remodeling4. In combination, PET/MRI systems allow for comprehensive imaging of the whole joint, including soft tissues and bone, which is necessary to study complex disease processes in OA5,6. This study aims to evaluate PET/MR knee imaging to detect and characterize osseous metabolic abnormalities and correlate PET radiotracer uptake with osseous abnormalities and cartilage degeneration observed on MRI7.Methods
For initial study, both knees of 22 subjects with knee pain or injury were imaged on a hybrid 3.0T Time-of-Flight PET-MRI system (GE Healthcare, Milwaukee, WI) following injection of 2-5 mCi of 18F-fluoride under IRB approval. A musculoskeletal radiologist identified volumes of interest (VOI) around bone abnormalities on MR images and scored bone marrow lesions (BMLs) and osteophytes using a MOAKS3 scoring system. Additionally, cartilage appearance adjacent to bone abnormalities was graded with an MRI-modified Outerbridge classifications. On PET standardized uptake values (SUV) maps, VOIs with SUV greater than 5 times the SUV in normal appearing bone were identified as high uptake VOI (VOIHigh). Differences in 18F-fluoride uptake between bone abnormalities, BML and osteophyte grades, and adjacent cartilage grades on MRI were identified using Mann-Whitney U tests. Additionally, 23 subjects with unilateral ACL tears and otherwise healthy contralateral knees(N=19) or bilateral ACL tears(N=4) were analyzed.Results and Discussion
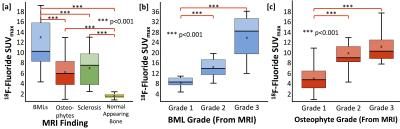
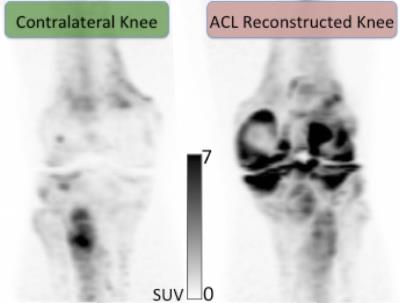
Static maximum 18F- fluoride PET standardized uptake values (SUVmax) in all subchondral bone lesions (BML, osteophytes, sclerosis) identified on MRI were significantly higher than that of normal appearing bone on MRI [p<0.001 for all](Figure 1). Furthermore, SUVmax was significantly higher in BMLs than in other lesions, and significant differences in PET uptake were observed between BML and osteophyte grades based on MOAKS3 (Figure 2). Of note, more than half of small, grade-1 osteophytes identified on MRI, often described as the earliest signs of OA, did not correlate with high 18F-fluoride uptake (SUVmax>5)(Figure 2b). This observation suggests that 18F-fluoride PET provides a quantitative measure to characterize these lesions and understand which are active in the progression of OA. Of significant interest, 37%(63/172) of high uptake regions on 18F-fluoride PET did not correspond to any abnormal findings on MRI (Figure 2c). As molecular changes often precede changes at the tissue level, this suggests that 18F-fluoride may serve as a marker of early bone remodeling changes that occurs before structural MRI damage is seen in the joint. Additionally, in subjects with unilateral ACL tears, a considerable increase in 18F- fluoride uptake was observed in the injured knee compared to the contralateral knee (Figure 3). ACL injuries are a known risk factor for development of OA with cartilage macromolecular changes observed as early as 1-year post injury8. 18F-fluoride PET, in combination with MRI, may be an ideal tool to simultaneously examine longitudinal changes in bone structure and metabolism.
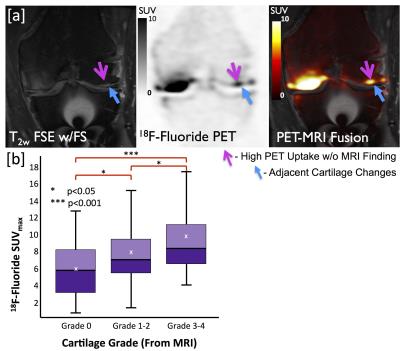
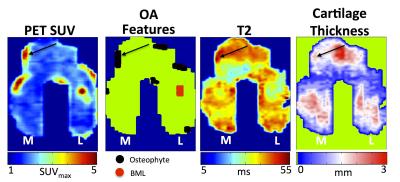
One of the biggest benefits of hybrid PET-MR imaging of OA is the ability to simultaneously evaluate spatial relationships across tissues. In addition to MRI bone findings, a trend was observed between increased 18F- fluoride PET uptake and increasing structural degeneration in the adjacent cartilage (Figure 4). This suggests that bone metabolism and late-stage degenerative cartilage changes are linked. Degradation of cartilage and subchondral bone are well-recognized features of OA. While these events are often studied in isolation, there is evidence that the bone–cartilage interface functions as a synergistic unit, with biochemical and molecular crosstalk between bone and cartilage9. 18F-fluoride PET, in combination with early MRI metrics of cartilage biochemistry10 such as T2, provides an optimal method to study bone-cartilage relationships in early OA (Figure 5). Additionally, other PET tracers, such as 18F-FDG, may provide complementary information about soft tissue inflammation, and could be utilized in combination to study OA degeneration in the entire joint.
Conclusion
PET/MRI can simultaneously assess multiple early metabolic and morphologic markers of knee OA across multiple tissues in the joint. Our findings suggest that PET/MR may detect metabolic abnormalities in subchondral bone, which appear normal on MRI. This approach offers a considerable advance for imaging of OA; including new markers of early disease and insights into the spatiotemporal progression of OA.Acknowledgements
This work was supported by a National Institute of Health (NIH) (Grant R01EB002524, K24AR062068) and research support from GE Healthcare.References
1. Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP, Suter LG, Losina E. The number of persons with symptomatic knee osteoarthritis in the United States: Impact of race/ethnicity, age, sex, and obesity. Arthritis care & research 2016.
2. Li X, Majumdar S. Quantitative MRI of articular cartilage and its clinical applications. J Magn Reson Imaging 2013;38(5):991-1008.
3. Hunter D, Guermazi A, Lo G, Grainger A, Conaghan P, Boudreau R, Roemer F. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis and Cartilage 2011;19(8):990-1002.
4. Czernin J, Satyamurthy N, Schiepers C. Molecular mechanisms of bone 18F-NaF deposition. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2010;51(12):1826-1829.
5. Torigian DA, Zaidi H, Kwee TC, Saboury B, Udupa JK, Cho ZH, Alavi A. PET/MR imaging: technical aspects and potential clinical applications. Radiology 2013;267(1):26-44.
6. Kogan F, Fan AP, Gold GE. Potential of PET-MRI for imaging of non-oncologic musculoskeletal disease. Quantitative Imaging in Medicine and Surgery 2016;6(6):756-771.
7. Kogan F, Fan AP, McWalter EJ, Oei EHG, Quon A, Gold GE. PET/MRI of metabolic activity in osteoarthritis: A feasibility study. Journal of Magnetic Resonance Imaging 2016:n/a-n/a.
8. Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, Ma CB, Majumdar S. Cartilage in Anterior Cruciate Ligament Reconstructed Knees: MR Imaging T1 and T2. Initial Experience with 1-year Follow-up. Radiology 2011;258(2):505.
9. Lories RJ, Luyten FP. The bone-cartilage unit in osteoarthritis. Nature reviews Rheumatology 2011;7(1):43-49.
10. Oei EH, van Tiel J, Robinson WH, Gold GE. Quantitative radiological imaging techniques for articular cartilage composition: Towards early diagnosis and development of disease-modifying therapeutics for osteoarthritis. Arthritis care & research 2014.
Figures