0027
Detection of intracranial vessel wall lesions using 7T MRI: patients with posterior circulation ischemia versus healthy controls1Radiology, University Medical Center Utrecht, Utrecht, Netherlands, 2Neurology and Neurosurgery, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
In this study presence and distribution of vessel wall lesions within the intracranial arteries of patients with recent posterior circulation ischemia and matched asymptomatic volunteers were assessed, using intracranial vessel wall MRI at 7T. Overall, vessel wall lesion presence and distribution were comparable between both groups. On arterial segment level, patients showed significantly higher lesion burden in the posterior cerebral artery, suggesting an association between posterior circulation lesion burden and ischemic events. Furthermore, a large amount of lesions showed contrast-enhancement, while the percentage of enhancing lesions was highest in the posterior circulation of the patient group.
Introduction
In the last decade, in vivo high field MRI (i.e. 3T and 7T) pulse sequences have been developed for direct visualization of the intracranial vessel wall.1 These techniques enable detection of vessel wall changes, including those that have not yet caused luminal narrowing.2 Assessment of presence and distribution of vessel wall lesions within the intracranial arterial tree has already been performed in patients with recent ischemia of the anterior cerebral circulation.3-5 Although ischemic stroke of the anterior circulation is most common, the posterior circulation still accounts for approximately 20-30% of all ischemic strokes.6 7 Therefore, the aim of the current study was to assess the presence of vessel wall lesions within the intracranial arteries of patients with recent posterior cerebral circulation ischemia, using intracranial vessel wall MRI at 7T. To put the vessel wall lesion burden of symptomatic patients in perspective, a direct comparison with age- and sex-matched asymptomatic volunteers was performed.Methods
Patients presenting with ischemic stroke or TIA of the posterior cerebral circulation, as well as age- and sex-matched volunteers without a history of cerebrovascular disease were included in this study. All subjects were scanned on a 7T whole-body system (Philips Healthcare) with a 32-channel receive coil and volume coil for transmission (Nova Medical). The imaging protocol included a high-resolution 3D T1-weighted magnetization-prepared inversion recovery turbo spin echo (MPIR-TSE) intracranial vessel wall sequence8 before and after contrast administration. Postcontrast vessel wall images were obtained to visualize potential enhancement of the arterial vessel wall. Two raters independently scored vessel wall lesions (number and location) and enhancement (present/absent) in all segments and proximal branches of the circle of Willis according to the method previously described3. A vessel wall lesion was defined as either a clear focal or more diffuse thickening of the vessel wall, as compared to the healthy contralateral or neighboring vessel wall.5 In case of disagreement, a consensus reading was performed with a third rater. Differences between groups were analysed with Pearson’s χ2 test or Mann-Whitney U test; for differences within groups the Wilcoxon signed-rank test was used.Results
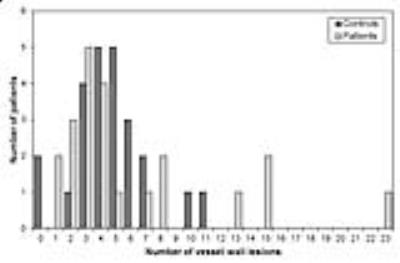
Presence and distribution vessel wall lesions (Table 1): In total 22 recently symptomatic patients (17 with stroke; 19 male; age 62±10 years) and 24 asymptomatic controls (20 male; age 60±12 years) were included for analysis. The mean number of vessel wall lesions per subject was 6.1 (range: 1-23) in the patient group, and 4.7 (range: 0-11) in the control group (p=0.76). Apart from three patients who had a relatively high number of vessel wall lesions, the distribution of vessel wall lesion burden between patient group and control group was comparable (Figure 1). Overall, in both groups, lesions occurred more often in the posterior circulation (64.7% vs. 59.8% in patients vs. controls) compared with the anterior circulation (respectively 35.3% vs. 40.2%; p=0.008 and p=0.046 for resp. patients and controls, and p=0.44 between groups), and there was no difference in lesion burden between left and right side of the circle of Willis (p=0.73 and p=0.12 for patients and controls, respectively). Regarding individual arterial segments, only the PCA showed significantly more vessel wall lesions in the patient group compared with the control group (p=0.038).
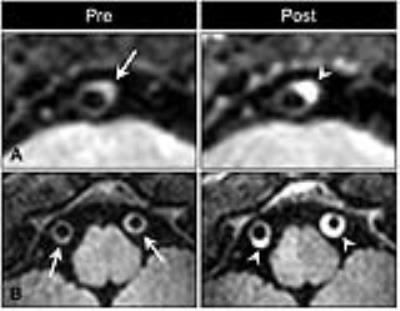
Enhancement (Figures 2 and 3): Contrast-enhancement occurred more often in vessel wall lesions of the patient group (65/133, 48.9%) compared with the control group (47/112, 42.0%), however, this difference was not significant (p=0.28). The percentage of lesions showing enhancement in the posterior circulation was higher in the patient group (52/86, 60.5%) compared with their anterior circulation (13/47, 27.7%; p<0.001), as well as the posterior circulation of the control group (31/67, 36.3%; p=0.08).
Discussion and conclusion
Vessel wall lesion presence and distribution were comparable between patients with recent posterior circulation ischemia compared with an age- and sex matched control group without cerebrovascular disease. In the PCA more vessel wall lesions were identified in the patient group. A large amount of lesions showed enhancement in the total study population, while the percentage of enhancing lesions was highest in the posterior circulation of the patient group. This might suggest an association of enhancement with (acute) ischemic stroke9; however, this enhancement could also represent vasa vasorum neovascularization that may have developed as a result of normal vessel wall thickening during ageing10. Future studies focusing on thickness variation and histological validation may shed light on the exact nature of this enhancement. In conclusion, intracranial vessel wall lesions can be found in both patients and matched asymptomatic volunteers. Patients showed significantly higher lesion burden in the PCA, suggesting an association between posterior circulation lesion burden and ischemic events.Acknowledgements
No acknowledgement found.References
1. Dieleman N, van der Kolk AG, Zwanenburg JJ, et al. Imaging intracranial vessel wall pathology with magnetic resonance imaging: current prospects and future directions. Circulation 2014;130(2):192-201.
2. Bodle JD, Feldmann E, Swartz RH, et al. High-resolution magnetic resonance imaging: an emerging tool for evaluating intracranial arterial disease. Stroke 2013;44(1):287-92.
3. van der Kolk AG, Zwanenburg JJ, Brundel M, et al. Intracranial vessel wall imaging at 7.0-T MRI. Stroke 2011;42(9):2478-84.
4. van der Kolk AG, Zwanenburg JJ, Brundel M, et al. Distribution and natural course of intracranial vessel wall lesions in patients with ischemic stroke or TIA at 7.0 Tesla MRI. Eur Radiol 2015;25(6):1692-700.
5. Dieleman N, van der Kolk AG, Zwanenburg JJ, et al. Relations between location and type of intracranial atherosclerosis and parenchymal damage. J Cereb Blood Flow Metab 2015.
6. Bamford J, Sandercock P, Dennis M, et al. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991;337(8756):1521-6.
7. Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Registry: analysis of 1,000 consecutive patients with first stroke. Stroke 1988;19(9):1083-92.
8. van der Kolk AG, Hendrikse J, Brundel M, et al. Multi-sequence whole-brain intracranial vessel wall imaging at 7.0 tesla. Eur Radiol 2013;23(11):2996-3004.
9. Gupta A, Baradaran H, Al-Dasuqi K, et al. Gadolinium Enhancement in Intracranial Atherosclerotic Plaque and Ischemic Stroke: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2016;5(8).
10. Portanova A, Hakakian N, Mikulis DJ, et al. Intracranial vasa vasorum: insights and implications for imaging. Radiology 2013;267(3):667-79.
Figures