0026
Intracranial vessel wall imaging in suspected cerebral vasculitis: evaluation of diagnostic value and treatment effects using 3T and 7T MRI1Radiology, University Medical Center Utrecht, Utrecht, Netherlands, 2Neurology, University Medical Center Utrecht, Utrecht, Netherlands, 3Images Science Institute, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
Cerebral vasculitis is a rare, but devastating disease that can lead to severe disability or death. Diagnosis is rather challenging, but for treatment purposes, an accurate diagnosis is crucial since different, more aggressive therapy is needed compared with non-inflammatory diseases. In the current study, we investigated the diagnostic value of intracranial vessel wall MRI at 3T and 7T in patients who were suspected of cerebral vasculitis. Our results show that intracranial vessel wall imaging at 3T and 7T MRI should be considered a promising non-invasive diagnostic tool to identify wall enhancement in patients with a suspicion of cerebral vasculitis.
Background and Purpose
Cerebral vasculitis is a rare, but devastating disease that can lead to severe disability or death.1,2 The clinical symptoms are broad and also seen in other non-inflammatory vessel wall diseases.3 Combined with the relatively low sensitivity of current diagnostic techniques like digital subtraction angiography (DSA) and brain biopsies, this makes diagnosis and differentiation rather challenging.3–5 For treatment purposes, however, an accurate diagnosis of vasculitis is crucial since different, more aggressive therapy is needed compared with non-inflammatory diseases.1 Intracranial vessel wall imaging is an emerging technique that may support the diagnostic process of this rare disease.6,7 With the addition of a contrast agent, vessel wall enhancement may be detected, providing information about inflammatory processes within the vessel wall.6,8–10 In the current study, we investigated the diagnostic value of intracranial vessel wall MRI at 3T and 7T in patients who were suspected of cerebral vasculitis on the basis of clinical signs and symptoms. The aim was to evaluate vessel wall changes i) between baseline and follow-up, ii) after immunosuppressive therapy and iii) to compare 3T and 7T vessel wall images.Methods
Ten consecutive patients with suspected cerebral vasculitis (mean age 49 years;8 males) were scanned at 7T MRI (Philips Healthcare) using a 3D T1-weighted Magnetization-Preparation Inversion-Recovery Turbo-Spin-Echo (MPIR-TSE) intracranial vessel wall sequence7 before and after contrast administration. A subset of seven patients also had a 3T MRI scan (Achieva, Philips Healthcare), including a transverse 3D T1-weighted Volumetric Isotropically-Reconstructed Turbo-spin-echo Acquisition (VIRTA) sequence11 after contrast administration only. Follow-up 7T MRI scans (median follow-up: 8 months) were obtained in six patients, five of whom received contrast agent. Five minutes before acquisition of the contrast-enhanced MPIR-TSE sequence, 0.1 mL/kg of a gadolinium-containing contrast agent (Gadobutrol, Gadovist 1.0 mmol/mL, Bayer Schering Pharma, Newbury, UK) was administered to the patients. Four patients were treated with immunosuppressive therapy, three of them also had a follow-up scan. Image analysis was performed with MeVisLab v2.5 (MeVis Medical Solutions AG, Bremen, Germany). Vessel wall lesions were scored per vessel segment on the 3T and 7T vessel wall images by two independent raters (ND and AK); consensus was reached in case of disagreement. Enhancement7,12 was scored on the 7T images by the same raters. Wilcoxon signed-rank tests were used to assess differences between baseline and follow-up and between 3T and 7T MRI. Dice Similarity Coefficient (DSC) and Intraclass Correlation Coefficient (ICC) were calculated for 3T and 7T MRI. Statistical significance was set at p<0.05.Results
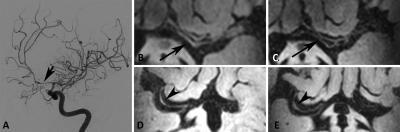
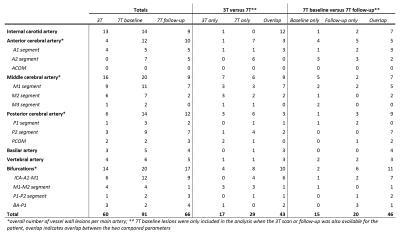
General characteristics: At baseline, 91 vessel wall lesions were found at 7T and 60 lesions at 3T MRI; 43 of these lesions overlapped (Figure 1). Statistical analysis showed no statistical differences between 3T and 7T lesion detection (p=0.08) (Table 1). After contrast administration, 44 (60%) of the vessel wall lesions enhanced at 7T in nine patients. A strong interrater reliability was found for both 3T (ICC 0.97, 95% CI: 0.802-0.994) and 7T (ICC 0.90, 95% CI: 0.698-0.963). Interrater agreement was good to strong for 3T (DSC 0.81) and 7T (DSC 0.74).
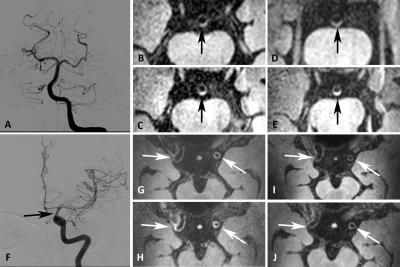
Follow-up and enhancement: By the end of the follow-up period, 66 vessel wall lesions were identified at 7T (p=0.40 vs baseline) (Figure 2 and Table 1). Of the 60 lesions that were eligible for enhancement analysis (one patient did not receive contrast), 16 lesions (27%) showed contrast-enhancement at follow-up, including 11 new enhancing lesions (Table 2). At follow-up, the no. of enhancing lesions decreased by 36% (16 vs 25), (p=0.11). A sub-analysis, including only those lesions that enhanced at baseline, revealed a statistically significant decrease in lesion enhancement between baseline (n=25) and follow-up (n=5) (80% reduction; p<0.0001). After treatment, enhancement was resolved in all, at baseline enhancing lesions (n=18) (Figure 3).
Discussion & Conclusion
Our results demonstrate reduced enhancement in patients treated with immunosuppressive agents, which could be promising for monitoring the dynamic inflammatory activity in cerebral vasculitis. Furthermore, our results suggest that arterial wall thickening and number of lesions can also be monitored overtime to investigate chronic damage caused by the inflammatory response. Both 3T and 7T were equally good at identifying lesions. Overall, Intracranial vessel wall imaging at 3T and 7T MRI should be considered a promising non-invasive diagnostic tool to identify enhancement in patients with a suspicion of cerebral vasculitis. It may help in decision-making with regard to treatment management, reduce over treatment in patients with pathologies resembling vasculitis, and may ultimately replace the necessity of invasive brain biopsies. However, for validation of this technique, it first has to be compared with brain biopsies to establish its definite role in the diagnosis and evaluation of cerebral vasculitis.Acknowledgements
This research was supported by the Netherlands Organization for Scientific Research (NWO) under grant n°91712322 and the European Research Council (ERC) under grant agreements n°637024.References
1. Hajj-Ali, R. A., Singhal, A. B., Benseler, S., Molloy, E. & Calabrese, L. H. Primary angiitis of the CNS. Lancet Neurol 10, 561–572 (2011).
2. Salvarani, C., Brown, R. D. & Hunder, G. G. Adult primary central nervous system vasculitis. Lancet 380, 767–777 (2012).
3. Birnhaum, J. & Hellmann, D. Primary Angiitis of the Central Nervous System. Arch Neurol 66, 704–709 (2009).
4. Salvarani, C. et al. Primary central nervous system vasculitis: Analysis of 101 patients. Ann. Neurol. 62, 442–451 (2007).
5. Hajj-Ali, R. A., Furlan, A., Abou-Chebel, A. & Calabrese, L. H. Benign angiopathy of the central nervous system: cohort of 16 patients with clinical course and long-term followup. Arthritis Rheum 47, 662–669 (2002).
6. Dieleman, N. et al. Imaging intracranial vessel wall pathology with magnetic resonance imaging current prospects and future directions. Circulation 130, 192–201 (2014).
7. van der Kolk, A. G. et al. Intracranial vessel wall imaging at 7.0-T MRI. Stroke. 42, 2478–84 (2011).
8. Mandell, D. M. et al. Vessel wall MRI to differentiate between reversible cerebral vasoconstriction syndrome and central nervous system vasculitis: preliminary results. Stroke 43, 860–862 (2012).
9. Pfefferkorn, T. et al. Black blood MRI in suspected large artery primary angiitis of the central nervous system. J. Neuroimaging 23, 379–83 (2013).
10. Saam, T. et al. High-resolution black-blood contrast-enhanced T1 weighted images for the diagnosis and follow-up of intracranial arteritis. Br J Radiol 83, e182-4 (2010).
11. Dieleman, N. et al. Qualitative evaluation of a high-resolution 3D multi-sequence intracranial vessel wall protocol at 3 tesla MRI. PLoS One 11, 1–11 (2016).
12. Swartz, R. H. et al. Intracranial arterial wall imaging using high-resolution 3-tesla contrast-enhanced MRI. Neurology 72, 627–634 (2009).
Figures