0022
The value of 7T in the clinical evaluation of epileptic patients with focal cortical dysplasia1State Key Laboratory of Brain and Cognitive Science, Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, Beijing, People's Republic of China, 2University of Chinese Academy of Sciences, Beijing, People's Republic of China, 3Xunanwu Hospital Capital Medical University, Beijing, People's Republic of China, 4Chinese PLA general hospital, Beijing, People's Republic of China
Synopsis
Focal cortical dysplasia (FCD) is defined as topical malformations of cortical development and often results in intractable epilepsy. However, many epileptic patients with FCD have not been diagnosed because of the lack of high-quality magnetic resonance imaging. 7T MRI, in comparison with 3T, is assessed in this study to allow better characterization of lesion details and detect previously unrevealed FCD abnormalities. The results of comparison were classified for an accurate and appropriate appraisal.
Introduction
Focal cortical dysplasia (FCD) belongs to the large spectrum of malformations of cortical development and is often related to intractable epilepsy submitted to surgical treatment. It is clinically important to accurately localize lesions. However, 16-43% of epileptic patients with FCD show negative results on conventional MRI system(1). In this work, 7T MRI with high spatial resolution and new tissue contrast mechanisms was utilized to better localize seizure foci within clinically reasonable time. Compared with 3T MRI, 7T MR imaging demonstrated improved visualization and more anatomical details of FCD and further detected previously unrevealed FCD lesions.Methods
Twenty patients (12 male, ages 13-42 years old) were scanned on a 7T research system (Siemens, Erlangen, Germany) with a volume transmit/32 channel receive head coil (Nova Medical). The study was approved by the Institutional Review Board of the Beijing MRI Center for Brain Research. The patients exhibited unclear or MRI-negative results at conventional 3T field strengths. 7T sequences including a high-resolution T1-weighted MPRAGE (0.6mm iso), WM-suppressed and GM/WM boundary–suppressed MPRAGE (0.7mm iso, TI=580ms/730ms) (2), MR2RAGE (0.5mm iso), 2D FLAIR (0.6*0.4*3mm3), T2-weighted TSE (0.3*0.3*2mm3), SWI (0.3*0.3*2mm3) and T2*-weighted GRE (0.21*0.21*1.5mm3) were performed. The 7T images were reviewed by an epileptologist with longstanding experience and compared with the corresponding routine sequences on conventional 3T MRI, which included T1- and T2-weighted, and 2D FLAIR images. The results of comparison were classified into three categories: equal (exhibiting similar results with 3T), better (providing more information of lesions) and groundbreaking (finding new lesions undetected by 3T).Results
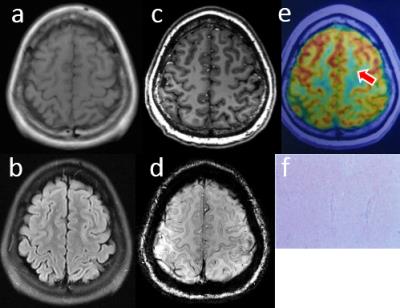
7T did not detect out any structural abnormalities in seven of the twenty patients (35%), who were also not previously revealed by conventional MRI. Although seizures were recorded in the patients using scalp video-electroencephalogram (EEG) or intracranial EEG, anatomical lesions related to epilepsy were not recognized from the images of 3T and 7T. This may be caused by subtle focus and particularity of pathologic characteristics. The patients were considered MRI-negative and needed further examinations. In figure 1, one patient (female, 26 years old) with MRI-negative results demonstrated low metabolism at the frontal lobe, which has been validated by intracranial EEG.
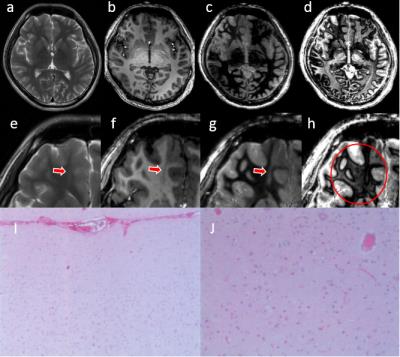
In 7 patients (35%), 7T provided better localization of foci and demonstrated more precise characterization of lesion details in comparison with conventional 3T MRI. Based on higher spatial resolution and better tissue contrast, 7T provided more information for diagnosis. Figure 2 showed the MRI results for one FCD patient (male, 24 years old). One blurred lesion was found in 2D T2-weighted and FLAIR images of 3T. The details were difficult to be observed and hard to be diagnosed. In comparison, 7T provided clearer lesion borders and detected more surrounding abnormalities. Pathological diagnosis demonstrated more subarachnoid small blood vessels and increased Dysmorphic Neurons and Balloon cells at focal cortices.
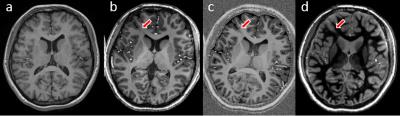
In six of
the 20 (30%) patients, 7T achieved breakthrough results and detected structural
abnormalities that had not been previously revealed by conventional 3T MRI. Besides
high SNR, high spatial resolution and better tissue contrast, new imaging
protocol at 7T, including WM-suppressed technique also contributed to the
ability of detecting FCD lesions. As indicated in figure 3, a new FCD lesion for
one female patient (19 years old) was revealed by T1 MPRAGE at 7T. And the new
imaging protocols, including MP2RAGE and the WM-suppressed sequence gave more clear
description for the lesion boundaries and details.
Discussions and Conclusions
7T MRI with high magnetic field strength was assessed as a potential clinical approach for patients with FCD epilepsy. There were some challenges including absent signals at the temporal lobe and deep brain regions caused by inhomogeneous B1 field, which would counteract the advantages of 7T at corresponding cerebral regions. This might lead to MRI-negative results for some patients at 7T. Of course, the improved spatial resolution and tissue contrast offered by 7T allowed more precise localization and characterization of FCD lesions. Higher resolution, better contrast and new protocols at 7T facilitated better depiction of FCD and detected previously unidentified subtle FCD abnormalities. Based on our findings, 7T MRI can offer better preoperative assessment and surgical planning for about 65% epileptic patients with FCD.Acknowledgements
We would like to thank Ms. Jing An (Siemens Shenzhen MR Ltd., China) for her technical assistance. This work was supported in part by Chinese MOST grants (2015CB351701, 2012CB825500), NSFC grant (91132302), and CAS grants (XDB02010001, XDB02050001).References
1. De Ciantis A, Barba C, Tassi L, et al. 7T MRI in focal epilepsy with unrevealing conventional field strength imaging. Epilepsia 2016;57:445–454.
2. Tourdias T, Saranathan M, Levesque IR, Su J, Rutt BK. Visualization of intra-thalamic nuclei with optimized white-matter-nulled MPRAGE at 7T. Neuroimage [Internet] 2014;84:534–545.
Figures