4142
Feasibility of Single Breath-hold Isotropic Voxel 129Xe MRI in Patients1Robarts Research Institute, London, ON, Canada, 2Medical Biophysics, Western University, London, ON, Canada, 3Division of Respirology, Department of Medicine, Western University, London, ON, Canada
Synopsis
Hyperpolarized 129Xe gas MRI has been established as an effective tool to investigate lung function in a number of pulmonary diseases. Improved 129Xe polarization techniques provide the opportunity to use a high-resolution 3D static ventilation image acquisition sequence (FGRE) in a 16-second breath-hold. Isotropic-voxel images were acquired in one healthy-volunteer and two patients with asthma; images were compared to coronal images acquired in two other patients with asthma. Isotropic images had sufficient SNR to analyze VDP. This proof-of-concept investigation establishes the feasibility of using an isotropic-voxel acquisition sequence in single breath-hold MRI of the lungs.
PURPOSE
Inhaled hyperpolarized gas MRI has been proven to be useful for the observation of and treatment planning for several pulmonary diseases including chronic obstructive pulmonary disease (COPD),1 asthma2 and lung cancer.3 Even after 20 years of developing hyperpolarized gas MRI,4 technological challenges have seriously limited its translation into clinical practice. Low SNR 129Xe images impede the development of many novel acquisition schemes that are highly sensitive to SNR,5 such as isotropic voxel static-ventilation imaging, accelerated multiple b-value diffusion-weighting MRI,6 and accelerated simultaneous collection of 129Xe gas and 129Xe within lung tissue/blood. The recent improvement in xenon polarization provides a way to develop advanced imaging methods previously not possible. This is especially critical for investigations in patients with asthma and COPD. We hypothesize that the isotropic-voxel, high-resolution 3D 129Xe static-ventilation image can be acquired in single 16 second breath-hold, with necessary and sufficient SNR to generate ventilation-defect-percent7 (VDP) estimates. Therefore, in this proof-of-concept evaluation, our objective was to demonstrate feasibility of this method in a small group of patients.METHODS
A healthy-volunteer and four asthma patients provided written informed consent to an ethics-board-approved study protocol and underwent spirometry and 129Xe MRI. Imaging was performed at 3.0T (MR750, GEHC, WI) using whole-body gradients (5G/cm maximum) and a commercial 129Xe quadrature-flex RF coil (MR Solutions, USA).8 Isotropic-voxel 129Xe static ventilation images were acquired using an axial plane 3D Fast Gradient Recall Echo (FGRE) sequence (TE/TR/initial-flip-angle=1.3ms/4.0ms/0.9o, variable-flip-angle,9 reconstructed matrix size=128x128x104 [axial view], pixel bandwidth=217Hz, FOV=40x40x32cm3, voxel size=3x3x3mm3). Traditional resolution xenon static-ventilation images were acquired using a coronal plane 3D FGRE sequence (TE/TR/initial-flip-angle=1.5ms/5.1ms/1.3o, variable flip angle, pixel bandwidth=122Hz, reconstructed matrix size=128x128x16, FOV=40x40x24cm3, voxel size=3x3x15mm3) as previously described.7 All images were acquired in breath-hold (<16 second) after inspiration of 1.0L of gas (129Xe/4He mixture) from functional-residual-capacity. Hyperpolarized 129Xe gas was obtained from a turn-key, spin-exchange polarizer system (Polarean 9820 129Xe polarizer).10 Image SNR was calculated for five central slices for each axial, coronal and sagittal view using a 10x10 region of interest inside a lung region of homogeneous signal and using the same 10x10 region of interest outside the lung where there was no lung signal.11 VDP was generated using a semi-automated segmentation algorithm as previously described.7RESULTS
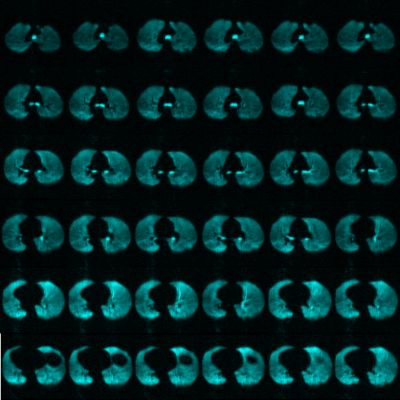
Figures 1 and 2 show isotropic-voxel static-ventilation images in axial and coronal views acquired from one healthy-volunteer and reconstructed from the same 3D k-space dataset. Table 1 summarizes demographic information as well as imaging results including SNR and VDP for three isotropic-voxel static-ventilation measurements (healthy-volunteer and two patients with asthma) and two traditional resolution static-ventilation measurements in two other patients with asthma. VDP for all five participants was less than 10%. Overall, SNR of the isotropic-voxel images was between 10-30 and SNR of the traditional resolution images was between 30-40. A coronal view SNR was normalized (SNRnorm) to the 129Xe volume and polarization for better understanding of the image quality limits; mean SNRnorm was 160 and 320 for the isotropic-voxel and traditional resolution images, respectively.DISCUSSION AND CONCLUSION
In this proof-of-concept study, we showed that 129Xe static-ventilation images can be acquired in a single 16 second breath-hold with sufficient SNR to analyze VDP. To the best of our knowledge, this is the first demonstration of 129Xe isotropic-voxel static-ventilation imaging with a 3D FGRE sequence. Normalized SNR for the isotropic-voxel images was approximately half that of the coronal non-isotropic images, however the voxel size was five times smaller. A previous investigation of 129Xe in patients with asthma where VDP was less than 10 reported SNR of 227 and this is consistent with our results. The SNR for the healthy-volunteer here was consistent with that previously-reported in a healthy-volunteer using a 3D Steady-State Free Precession isotropic-voxel acquisition with larger voxels (4.2x4.2x4.2mm3), a larger xenon dose (1.0L, 86% enriched 129Xe at 35% polarization) and greater flip angle (10o).12 Observed variation in the isotropic-voxel image SNR (healthy-volunteer vs. asthma patient-2) could be attributed to variation of the RF coil sensitivity caused by different patient sizes. A rigid and more homogenous coil13 combined with a phased-receive-array14 could substantially improve isotropic-voxel image quality and potentially replace the isotopically-enriched 129Xe with the natural-abundant xenon15 and consequently, reduce the cost of 129Xe MRI for patients. This study demonstrates the feasibility of isotropic-voxel MR imaging of the lungs within a single breath-hold scan.Acknowledgements
No acknowledgement found.References
1. Kirby, M. et al. Radiology 273, 887-896 (2014).
2. Svenningsen, S. et al. Am J Respir Crit Care Med (2018).
3. Hoover, D. A. et al. BMC Cancer 14, 934 (2014).
4. Albert, M. S. et al. Nature 370, 199-201 (1994).
5. Rao, M. R. et al. Radiology 286, 659-665 (2018).
6. Westcott, A. et al. J Magn Reson Imaging (2018).
7. Svenningsen, S. et al. J Magn Reson Imaging 38, 1521-1530 (2013).
8. Kaushik, S. S. et al. Magn Reson Med 75, 1434-1443 (2016).
9. Ouriadov, A. V. et al. MAGMA 22, 309-318 (2009).
10. Kaushik, S. S. et al. Magn Reson Med 65, 1154-1165 (2011).
11. Dominguez-Viqueira, W. et al. Magn Reson Med 66, 1400-1404 (2011).
12. Norquay, G. et al. Proceedings of the 25th Annual Meeting of ISMRM, Hawaii, USA, 2140 (2017).
13. Farag A et al. In Proceedings of the 20th Annual Meeting of ISMRM, Melbourne, Australia, 1233 (2012).
14. Chang, Y. V. et al. Magn Reson Med 73, 1609-1614 (2015).
15. Stewart, N. J. et al. Magn Reson Med 74, 346-352 (2015).