4094
Quantitative Pulmonary Ventilation Imaging in Patients with Cystic Fibrosis using breath-hold 3D-UTE at 3T1Department of Diagnostic and Interventional Radiology, University Hospital Würzburg, Würzburg, Germany, 2Department of Pediatrics, Universtiy Hospital Würzburg, Würzburg, Germany, 3Application Development, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
We demonstrate first results of breath-hold 3D-UTE MRI for ventilation imaging in CF patients. Ten patients underwent 3D-UTE MRI of the lungs. Data were acquired in breath-hold for 5 different breathing states, in order to obtain information regarding the ventilation. 3D-UTE MRI provided sufficient morphologic image quality for the detection of structural lung disease and site-resolved information regarding pulmonary ventilation. Ventilation measurements correlated well with parameters of conventional lung function testing and were in accordance with pulmonary ventilation measured with techniques published recently. The technique could be an innovative method able to enhance diagnosis and monitoring of structural lung disease.
Introduction
Low proton density in the lungs, fast signal decay and respiratory motion are well known problems in pulmonary magnetic resonance imaging (MRI). Recently, ultrashort echo time (UTE) sequences have been introduced in musculoskeletal imaging and were adopted and evolved for pulmonary MRI in order to accelerate the readout and hence to overcome the fast signal decay in the lungs (1-3). According to recent work, UTE imaging of the lung delivers radiation free CT-like depiction of lung morphology (4). By means of dynamic acquisitions with several breathing states, spatially resolved quantitative pulmonary ventilation (QV) can be determined adding valuable information for diagnosis and monitoring of structural lung disease (2,3). In this work, we demonstrate first results of multiple breath-hold 3D-UTE MRI for pulmonary ventilation imaging in patients with cystic fibrosis.Methods
Ten patients with cystic fibrosis underwent functional 3D-UTE MR imaging of the lungs at 3 Tesla (Magnetom Prisma, Siemens Healthcare, Erlangen, Germany). A prototypical UTE Spiral VIBE technique employing a 3D stack of spirals trajectory with dual-density spiral gradient waveforms (5) and SPIRiT reconstruction (6) was used for UTE imaging. The scan parameters were as follows: TE = 0.05ms; TR = 2.35ms; flip angle = 5°; in-plane resolution = 2.3mm x 2.3mm; slice thickness = 2.3mm; number of spiral readouts per partition = 132; iPAT factor = 2; number of partitions = 118 ± 12, breath-hold time = 14-19 seconds (depending on individual thoracic volume). Data were acquired in breath-hold for 5 different breathing states between inspiration and expiration, in order to obtain functional information regarding the ventilation. For calculation of ventilation maps, the 3D-images of the different breathing states were subsequently registered to the 3D-image of a single intermediate breathing state (7). Segmentation of the lungs was performed semi-automatically to obtain QV values as proposed earlier (2,8,9). Also, the air volume fraction (AVF) η of the lungs was estimated from a single breathing state on a voxel by voxel basis according to the following equation
$$ \eta \approx 1 - \frac{S_p}{S_{p,blood} } $$
where Sp denotes the signal in the pulmonary parenchyma and Sp,blood the signal of pure blood under the approximation of a pure proton density weighted dataset and that the blood pool consisting of 100% water. Values are presented as mean ± standard deviation for the whole lung. Finally, QV measurements were correlated to parameters of conventional lung function testing.
Results
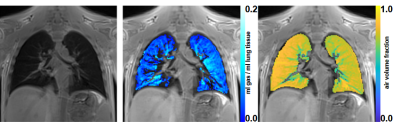
Figure 1 provides a representative morphologic image and color-coded QV and AVF maps of the lungs acquired with 3D-UTE MRI in a CF subject. The technique provides sufficient morphologic image quality to assess significant change in lung structure. Color-coded ventilation and air volume fraction maps allow for site-resolved assessment of these functional parameters. Mean QV in the patients with CF was 0.09±0.5 ml gas / ml lung tissue, which is in accordance with values of CF patients investigated with 2D-FLASH-based SENCEFUL-MRI, as published earlier (8,9). QV values as measured by 3D-UTE MRI correlated significantly with several lung function parameters. For vital capacity a spearman correlation coefficient of r=0.8 (p<0.01) was observed. Correlation to the forced expiratory volume in one second (FEV1), which is a marker for obstruction was r=0.8 (p<0.01). Finally, the measured mean AVF of the lungs was 0.75±0.04 for CF patients.Discussion
3D-UTE MRI provides sufficient morphologic image quality for the detection of structural lung disease and site-resolved functional information regarding pulmonary ventilation within short breath-holds. QV measurements correlated well with parameters of conventional lung function testing and were in accordance with pulmonary ventilation measured with techniques published recently. A limitation of the presented approach with respect to its routine clinical application is the need for patient´s compliance regarding the required breath-hold. In case of interrupted breath-holds, respective images may suffer from motion artifacts ultimately causing incorrect QV values.Conclusion
Functional MRI using 3D-UTE MR allows for simultaneous assessment of lung structure and ventilation parameters within a single examination free of contrast agents or radiation exposure. Therefore, the technique could be an innovative method able to enhance the diagnosis and monitoring of structural lung disease. In comparison to proton MRI techniques for ventilation measurements proposed earlier, 3D-UTE MRI provides images with higher resolution within shorter acquisition times.Acknowledgements
No acknowledgement found.References
- Qian Y, et al. Acquisition-Weighted Stack of Spirals for Fast Echo Time MR Imaging. Magn Reson Med. 2008 Jul;60(1):135-45
- Mendes Pereira L, et al. UTE‐SENCEFUL: first results for 3D high‐resolution lung ventilation imaging. Magn Reson Med. 2018; ePub ahead of print.
- Mendes Pereira L, et al. Self-gated ultra-short echo time lung MRI for quantitative ventilation assessment. Proc. Intl. Soc. Mag. Reson. Med. 25(2017); 3317.
- Ohno Y, et al. Pulmonary high-resolution ultrashort TE MR imaging: Comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. J Magn Reson Imaging 2016 43(2):512-532.5.
- Meyer CH, et al. Dual-density and parallel spiral ASL for motion artifact reduction. Proc. Int. Soc. Mag. Reson. Med. 19(2011);3986.
- Mugler JP, et al. Accelerated Stack-of-Spirals Breath-hold UTE Lung Imaging. Proc. Intl. Soc. Mag. Reson. Med. 25(2017);4904.
- Kroon DJ, et al. In IEEE International Symposium on Biomedical Imaging (ISBI): From Nano to Macro. 2009, 10814189.8.
- Veldhoen S, et al. Self-gated Non-Contrast-enhanced Functional Lung MR Imaging for Quantitative Ventilation Assessment in Patients with Cystic Fibrosis. Radiology 2016;283:242–251.9.
- Fischer A et al. SElf-gated Non-Contrast-Enhanced FUnctional Lung imaging (SENCEFUL) using a quasi-random fast low-angle shot (FLASH) sequence and proton MRI. NMR Biomed. 2014;27:907–17.