4089
MultiVane Technique at 1.5T Improved the Quality of Lung MRI: Comparison with Routine T2-Weighted MRI and CT Imaging1Radiology, The Longhua Hospital of Shenzhen, Shenzhen, China, 2Graduate School, Medical College of Nanchang University, Nanchang, China, 3Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, GA, United States, 4Department of Respiration, The Longhua Hospital of Shenzhen, Shenzhen, China
Synopsis
Radiation-free MRI with MultiVane motion correction technique improved the lung MR imaging quality with satisfactory quality compared to routine T2 weighted imaging or CT imaging. In this study, MultiVane lung MRI protocol provided diagnostic performance acceptable in detection of several common lung abnormalities with a good agreement to the findings obtained in routine clinical CT examinations, especially to identify caseation or liquefactive necrosis. However, MRI is less desirable to detect the nodules with calcification. The current lung MRI with non-radiation is feasible. It offers a promising alternative to the clinical standard CT in diagnosis and characterization of pulmonary diseases.
Introduction
MRI allows for radiation-free lung imaging, but lung MRI did not apply widely in clinic due to the technical challenges in low signal and sensitivity in motion control [1,2]. In this study, we used MultiVane (MV) motion correction technique [3] to improve the quality of lung MRI. It allowed us to obtain comparable performance with CT in pulmonary lesions detection and characterization.Materials and Methods
Ten healthy participants were enrolled to verify the optimized MRI protocol using the comparison of T2-MV and routine T2-Fast Spin Echo (FSE) sequences with respiratory triggering and free breathing at 1.5T MR scanner (Philips Achieva). The main MRI parameters included TE of 85/100 ms, TSE factor = 33, flip angle = 180/90° and phase resolution = 80% with slice thickness of 5 mm, field of view (FOV) = 400 × 400 mm, matrix size = 308 × 308, with free breathing. For respiratory triggered scan, actual TR was determined based on respiratory rhythm of the subject, which was typically in the range of 2,000-4,000 ms. T1-weighted spin echo sequence was not included in order to shorten acquisition time and simplify the lung MRI protocol. 63 patients with pulmonary tuberculosis (TB) (age = 39 ± 15 years, 50 males, 13 females) were recruited in this study. All routine chest CT images for comparison of computed tomography (CT) were obtained prior to the MRI exam. Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were calculated in selected regions of interesting (ROIs) for evaluation of lung MR imaging quality. Signal intensities (SI) were measured in selected ROIs with normal pulmonary parenchyma (SInormal) and the latissimus dorsi muscle (SImuscle). Then they were compared with background standard deviation (SD) in the same slice. SNR was then computed using the formulas: SNR = SInormal/SD and CNR = SImuscle - SInormal/SD. Two radiologists double-blinded evaluated all images quality and pulmonary lesions on the same workstation. Image quality was rated based on the severity of artifacts using a four-point scoring [4]. The lower score indicated the higher image quality. Lesions detection in MRI were compared to those in CT. A two-tailed, paired t-test was used to compare the difference of SNR and CNR in MV and routine T2 weighted MR imaging using SPSS (V19.0, IBM). A value of P < 0.05 was considered statistically significant. Cohen's kappa (κ value) was used to evaluate lung MR-CT image findings agreement.Results and Discussion
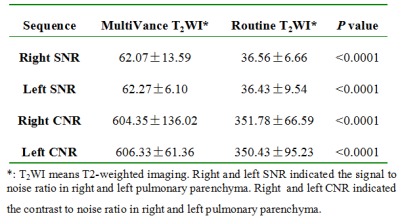
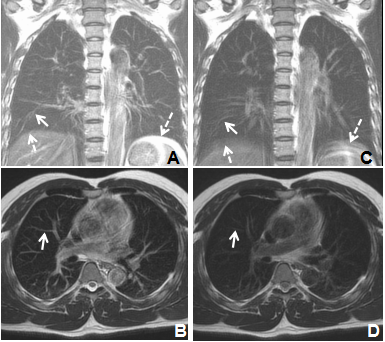
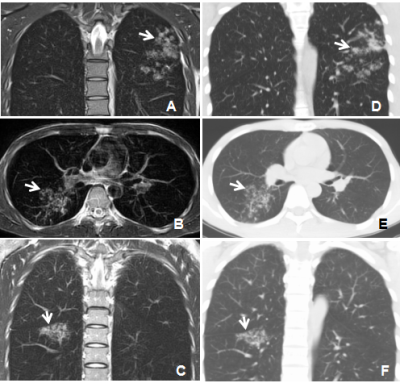
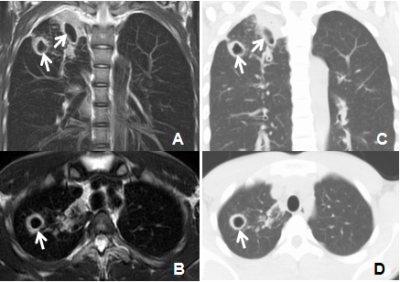
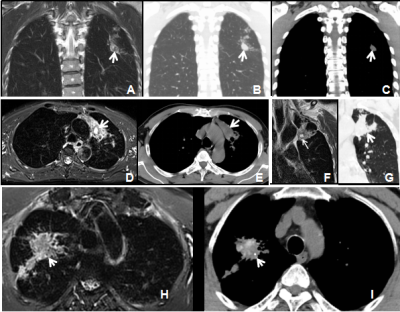
Our results showed MV technique significantly improved the lung MR image quality with reduced respiratory and cardiac motion artifacts in either normal pulmonary structures (Figure 1) or lesions. Both SNR and CNR of pulmonary parenchyma were increased significantly in MV T2-weighted imaging (Table 1) comparing to those of routine T2-weighted TSE imaging (P < 0.0001). Lung MR images with satisfactory quality were obtained in 63 subjects with pulmonary TB with 1 score (n = 31), 2 scores (n = 24), 3 scores (n = 8), and no case with 4 scores in MV T2-weighted imaging. Image with the lower score indicated the better imaging quality. Diagnostic information from images obtained in MV technique-implemented MRI has excellent agreement with those from CT in detection of several common lung abnormalities (κ = 0.88-1) in identifying tree-in-bud sign, interstitial change, consolidation (Figure 2), and cavitation (Figure 3). Current lung MRI was better to identify caseation or liquefactive necrosis (Figure 4A-4G), but it was not sensitive to detect or identify the lesions with calcification (Figure 4H-4I).Conclusions
MV technique-implemented T2-weighted imaging of the lung is a promising approach to improve image quality, which leads to increased detection and characterizing of different pulmonary lesions with different signal features in pulmonary TB.Acknowledgements
No acknowledgement found.References
1. Schloß, M., et al., Magnetic Resonance Imaging of the Lung as an Alternative for a Pregnant Woman with Pulmonary Tuberculosis. Journal of radiology case reports, 2015. 9(5): p. 7.
2. Ekinci, A., et al., MRI of pneumonia in immunocompromised patients: comparison with CT. Diagnostic and interventional radiology (Ankara, Turkey), 2016.
3. Rizzi, E.B., et al., Detection of Pulmonary tuberculosis: comparing MR imaging with HRCT. BMC Infect Dis, 2011. 11: p. 243.
4. Eibel, R., et al., Pulmonary abnormalities in immunocompromised patients: comparative detection with parallel acquisition MR imaging and thin-section helical CT. Radiology, 2006. 241(3): p. 880-91.
Figures