3670
Enhanced Value and Diagnostic Utility in Musculoskeletal MRI Using ZTE1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States
Synopsis
Zero Echo Time (ZTE) MRI affords CT-like positive contrast visualization of bone This study highlights instances in which ZTE imaging proved clinically useful as an adjunct to standard-of-care MRI in diagnosis and treatment of musculoskeletal injuries. Cases are presented in which patient circumstances (pregnancy, age, prior imaging, etc.) coupled with the underlying pathology resulted in added diagnostic, safety, monetary, and/or temporal value for the patient or care team. This study coupled with our prior work indicates that ZTE imaging can provide a suitable alternative to CT and, in certain circumstances may in fact, be preferable.
Introduction
Visualization of soft tissues with sufficient contrast and spatial resolution for the assessment of musculoskeletal disorders is readily achievable with magnetic resonance imaging (MRI). However, direct visualization of bone in standard MR pulse sequences is hindered by short transverse tissue relaxation times (T2) in osseous tissue. Zero Echo Time (ZTE) MRI is a pulse sequence capable of detecting the sparse, rapidly decaying MR signal in bone and has been employed in several musculoskeletal contexts including shoulder, cervical spine, ankle and hip,1-4 as well as for signal attenuation correction in PET imaging of the brain.5,6 Following appropriate post-processing to invert contrast,5,6 ZTE renders images with flat contrast for soft tissues and displays bone as hyperintense, similar to CT (see figures).
This study reviewed cases for which ZTE imaging was performed at our site under prior studies or physician requests and in which patients’ circumstances (age, pregnancy status, frequency of follow-up, repeat imaging, etc.) underscored the utility of ZTE bone imaging in adding value to the ordered standard-of-care (SOC) MRI. Diagnostic, safety, convenience, financial, and temporal values were considered. As the ZTE pulse sequence is a prototype, added values are stated as hypothetical and ZTE was ordered as an adjunct to each physician’s existing standard-of-care without presumption of any benefit. The objective of this study is to highlight examples in which ZTE imaging would likely have added value if employed as standard-of-care in diagnosis and visualization of osseous injury or disease.
Methods
Under IRB approval and informed written consent/assent, our radiology department has performed ZTE series in > 470 exams to date, including 30 juveniles (9-17 years) and 2 pregnant females. All patients were recruited through physician referral into the study or from our department’s radiology schedule, under IRB approved HIPAA waiver. Image series were collected on 1.5T or 3.0T scanners (Optima MR450W and Discovery MR750, GE Healthcare, Waukesha, WI) using standard patient positioning and commercial anatomy-specific coils (Invivo, Gainesville, FL or GE Healthcare), with the following scan parameters: TR: 300ms, flip angle: 1°, receiver bandwidth: ±62.5 kHz, matrix size: 320, slice thickness: 0.8-1.5 mm, scan time: 4-6 min, field-of-view (FOV): 10-32cm.Results
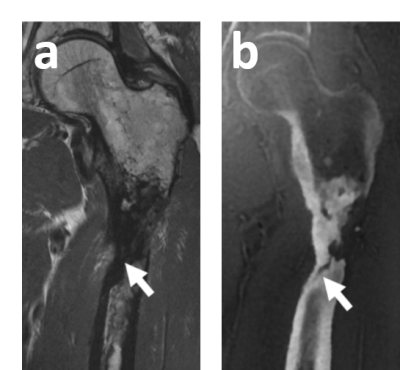
Of the ZTE exams performed at our site, 37 were used diagnostically, including 23 physician requests. Figures 1-3 show examples in which value was added to SOC MRI by including ZTE. Figure 1 shows a distal patellar avulsion wherein the extent of displacement is not clear in SOC MRI but readily seen on ZTE. Further, the lateral (image left) avulsed fragment is obscured in SOC MRI. Figure 2 shows comminuted malleolar fractures in which multiple bone fragments are readily apparent on ZTE. As this patient was pregnant (26wks), CT was inadvisable but ZTE provided necessary osseous detail for procedure planning. Figure 3 shows a femur after implant removal due to infection and subsequent periprosthetic fracture. This patient’s care included two SOC MRI exams 10 days apart to which ZTE was added. Sufficient osseous detail was afforded to visualize the persistent fracture deformities, obviating need for CT. Having undergone CT four months prior, this patient was spared further ionizing radiation doses, had CT been performed instead.Discussion
Cases included herein are examples of circumstances in which ZTE can complement standard MRI in the detection of clinically relevant osseous detail. Of greatest import in discussing value are quality of patient care and patient safety. Additional caveats to the application of ZTE imaging include that it is susceptible to metal artifact, and while pediatrics is an appropriate application of MRI to obviate radiation exposure from CT, some pediatric patients may be too young to remain still for the duration of the ZTE sequence (typically 4-6 minutes) without anesthesia.
Despite these limitations, our prior works1-4 have shown strong diagnostic agreement between CT and ZTE, suggesting that ZTE may serve as a substitute in certain instances. In these occasions ZTE is sufficiently equivalent to CT for given pathologies, enabling accurate diagnosis while eliminating ionizing radiation dose, especially critical in pediatric or pregnant patients. Of further benefit, ZTE renders a familiar ‘CT-like’ positive contrast for bone tissue, providing images more directly and intuitively interpretable by non-radiologists. Beyond quality of care, safety, and utility, ZTE imaging can save the patient/insurer money in these instances where MRI and CT would have been required. Further, the patient may save the time cost associated with an additional imaging appointment.
Acknowledgements
Hospital for Special Surgery maintains an institutional research agreement with GE HealthcareReferences
- Breighner et al. 2018, Radiology 286(3).
- Argentieri et al. 2017, Spine 43(13).
- Sahr et al. 2017 ISS Meeting.
- Breighner et al. ISMRM 2018.
- Sekine et al. 2016, J Nucl Med 57(12).
- Delso et al. 2015. J Nucl Med 56(3).
Figures