2886
Simultaneous MR Neurography and T2 Mapping (SHINKEI Quant) for Quantitative Evaluation of Lumbar Nerve Roots in Patients with Low Back Pain.1Radiology, Eastern Chiba Medical Center, Chiba, Japan, 2Division of Health Sciences, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Japan, 3Philips Japan, Tokyo, Japan, 4Orthopaedic Surgery, Eastern Chiba Medical Center, Chiba, Japan, 5General Medical Services, Chiba University Graduate School of Medicine, Chiba, Japan, 6Faculty of Health Sciences, Institute of Medical, Pharmaceutical and Health Sciences, Kanazawa University, Kanazawa, Japan
Synopsis
This study was to investigate the clinical utility of SHINKEI-Quant ( simultaneously acquire MR neurography and T2 mapping by further optimizing the improved motion-sensitized driven-equilibrium (iMSDE) preparation) for evaluation of lumbar nerve roots in patients with low back pain.
PURPOSE
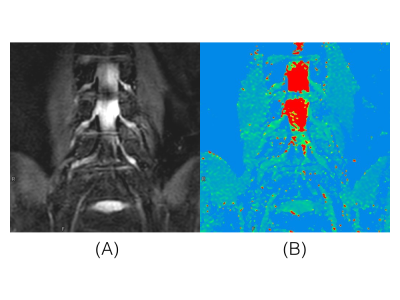
MR neurography achieves selective depiction of peripheral nerves and detect pathological changes related to neuropathies as a signal abnormality1-4. Hitherto, several studies have reported that the T2 assessment may offer functional information about the nerve injuries5-7. Thus, quantitative evaluation by using T2 value might be clinically useful to estimate the effect of treatment and/or to determine the prognosis. Recently, a new sequence (SHINKEI-Quant) was developed that could simultaneously acquire MR neurography and T2 mapping by further optimizing the improved motion-sensitized driven-equilibrium (iMSDE) preparation8 (Fig.1). In previous study, it was reported that evaluation of chronic inflammatory demyelinating polyradiculoneuropathy using SHINKEI-Quant9,10. We thought that this method can also be useful for assessment of low back pain patients. The purpose of this study was to investigate the clinical utility of SHINKEI-Quant for evaluation of lumbar nerve roots in patients with low back pain.METHODS
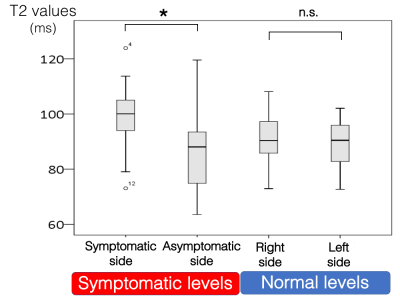
All subjects were examined with 3.0T whole-body clinical system (Ingenia CX, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects. Lumbar nerve roots of 15 patients who have low back pain and unilateral neurological symptoms were examined using SHINKEI-Quant. We visualized MR neurography and evaluated T2 values of bilateral nerve roots at normal levels and symptomatic levels (Fig.2). Imaging parameters for SHINKEI-Quant were; Coronal, voxel size=1.34*1.49*4.00mm3, FOV=300×300mm2, TR=2200ms, TE=1st 35, 2nd 70ms, fat suppression=SPAIR and total acquisition time=6m36s.RESULTS AND DISCUSSION
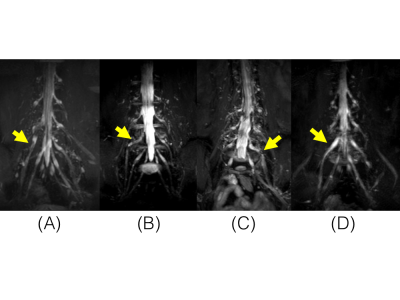
MR neurography using SHINKEI-Quant well depicted lumbar nerve roots more distally to extraforaminal area at normal levels, and indicated abnormalities such as morphological defect, deformation, narrowing and swell at symptomatic levels (Fig.3). There was no difference of average T2 values at normal levels. At the symptomatic level, average T2 values of symptomatic side were significantly higher than those of asymptomatic side (Fig.4). Since SHINKEI-Quant is based on turbo spin echo sequence and is less sensitive to distortion unlike to EPI, it might be high measurement accuracy of T2 values. Therefore, T2 assessment using SHINKEI-Quant might be helpful to determination of prognosis and estimation of treatment effect due to nerve injuries.CONCLUSION
SHINKEI-Quant could simultaneously acquire MR neurography and T2 mapping. This quantitative sequence might be helpful to quantitatively assess for evaluation of lumbar nerve roots in patients with low back pain.Acknowledgements
No acknowledgement found.References
[1] Filler AG, et al. Application of magnetic resonance neurography in the evaluation of patients with peripheral nerve pathology. J Neurosurg. 1996;85:299-309.
[2] Does MD, et al. Multiexponential T2 relaxation in degenerating peripheral nerve. Magn Reson Med. 1996;35:207-13.
[3] Aagaard BD, et al. MR neurography. MR imaging of peripheral nerves. Magn Reson Imaging Clin N Am. 1998;6:179-94.
[4] Britz GW, et al. Carpal tunnel syndrome: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery. 1995;37:1097-103.
[5] Shen J, et al. MR neurography: T1 and T2 measurements in acute peripheral nerve traction injury in rabbits. Radiology. 2010;254:729–738
[6] Zhang X, et al. MR imaging and T2 measurements in peripheral nerve repair with activation of Toll-like receptor 4 of neurotmesis. Eur radiol. 2014;24:1145-1152.
[7] Cha JG, et al. Median nerve T2 assessment in the wrist joints: preliminary study in patients with carpal tunnel syndrome and healthy volunteers. J Magn Reson Imaging. 2014;40:789-795.
[8] Yoneyama M, et al. SHINKEI Quant: Simultaneous Acquisition of MR neurography and T2 Mapping for Quantitative Evaluation of Chronic Inflammatory Demyelinating Polyneuropathy. Proc Intl Soc Mag Reson Med. 2016;24:1322.
[9] Hiwatashi A, et al. Simultaneous MR neurography and apparent T2 mapping in brachial plexus: Evaluation of patients with chronic inflammatory demyelinating polyradiculoneuropathy. Magn Reson Imaging 55 (2019) 112–117
[10] Hiwatashi A, et al. lumbar plexus in patients with chronic inflammatory demyelinating polyradiculoneuropathy: evaluation with simultaneous T2 mapping and neurography method with SHINKEI. Br J Radiol 2018; 91: 20180501.
Figures