2857
Towards the development of a microstructural model for Brain tumours1Clinical Imaging Sciences Centre, Brighton and Sussex Medical School, Brighton, United Kingdom, 2Neuroradiology Unit and CERMAC, Vita-Salute San Raffaele University and IRCCS San Raffaele Scientific Institute, Milan, Italy, 3Department of Computer Science, University College London, London, United Kingdom
Synopsis
While several multi-compartment models of diffusion have been developed to describe the healthy neural tissue, most of these models fail in the presence of tumours, because they are unable to capture their heterogeneity. By contrast, models of diffusion able to quantify histologic features of colorectal and prostate tumors in vivo have been proposed. Here we combine the sensitivity of these models to tumour histology and the ability of multi-compartment models of dMRI in the brain to describe the complexity of the neural tissue.
Introduction
Diffusion MRI (dMRI) is sensitive to tumour pathology, and can reflect altered cellularity. The dMRI signal can be modelled as a function of parameters such as the cell diameter and density, and extracellular volume (eg. 1), and perform well in differentiating benign and cancer regions (2) in body tumours. Their translation to brain tumours (eg. 3) is challenging because they do not capture the complexity of brain tissue, particularly with infiltrating masses, where additional compartments, accounting for the anisotropy and orientation dispersion of neural fibers, are needed. In addition, typically these models do not explicitly model free water, and thus tend to fail in the presence of extensive oedema (4). In this proof-of-concept study, we propose a model of dMRI within brain tumours. Our simplest model combines an isotropic restricted compartment (representing tumour cells) with an anisotropic hindered compartment (parenchyma) and free isotropic diffusion (for free water). We evaluate the performance of this model in 5 tumours with different grades, investigating its suitability to describe the signal in the core of the tumours, and the peripheral areas of the tumours, with the ultimate aim of providing biomarkers for tumour characterization and grading.Methods
Patients’ clinical data
Data were collected from 5 patients (4 males; median age=64 years; range=23-70 years); patients details and their histopathological diagnosis according to the new WHO 2016 brain tumor classification are shown in Table 1. , Patients 1-3 had WHO-III astrocytoma IDH-wt (wild-type) with infiltrative oedema, patient 4 had a secondary tumor lesion (metastasis from melanoma), with purely vasogenic oedema, and patient 5 had WHO-II astrocytoma (IDH-wt).
MRI imaging protocol
MRI was acquired at 3T (ingenia CX, Philips Healthcare). A series of 10 dMRI scans were acquired, each along 3 orthogonal diffusion-encoding directions varying the TE, the diffusion gradient amplitude (G), duration (δ), and separation (Δ). A b0 image was acquired for each TE. Finally we acquired a two-shell dMRI data set with b=711 (38 directions) and b=3000s/mm2 (63 directions), respectively, and TE=78ms. Twelve b0 images were also collected with the same TE. Additionally, 3D-FLAIR images and post-contrast 3D-T1 weighted images were acquired. Regions of interest (ROI) masks for the whole tumour were segmented on 3D-FLAIR images and for the tumour core on post-contrast 3D-T1 images, in order to outline the core and the periphery of the tumours (Figure 1).
Tissue model and fitting for the DWI data
The model characterizes the diffusion signal such that the total signal STotal within each voxel is the weighted sum of the signal from each compartment:
$$$S_{Total} = fic\star{S_{Sphere}} + fn\star{S_{Tensor}} +fiso\star{S_{Ball}}$$$
Where: SSphere is the signal from the tumour intra-cellular tissue (restricted water), STensor is the signal from the neural tissue, SBall is the signal from the free water, fic, fn and fiso are the volume fractions of the intra-cellular, neural tissue and free water, respectively. Details about the Sphere, Tensor and Ball models can be found in (4,5). For this proof-of-concept study we fixed the diffusivity within compartments: the intracellular diffusivity (di), and the free water diffusivity (diso) to 1*10-9 and 3*10-9 m2/s, respectively. So the following parameters were estimated fic, fn, R (cell radius)). The normalization constant and T2 were also fitted for all models to account for the variable TE. The free water volume fraction fiso was was calculated as: fiso = 1-( fic + fn ).
Results
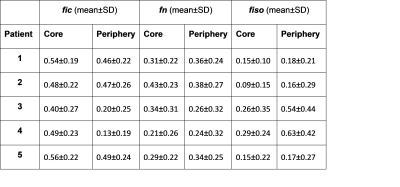
Voxel-wise maps of the volume fractions of the tumour intra-cellular tissue, neural tissue and free water for both the core and tumor regions as shown in figure 2 and figure 3. Table 2 details the mean values and standard deviation of these parameters.Discussion and conclusions
The results indicate that this model performs well in differentiating core and periphery, particularly in cases such as patient 4 (metastatic tumour). The lack of a vascular compartment is of course a limitation which might explain the high cellularity obtained in patient 5. In general, these data suggest that this may be a promising model particularly for infiltrating tumour with abundant oedemas. We are looking into the feasibility of including a vascular compartment, and separate intra-neurite and extra neurite compartments. This will render the model very complex mathematically and we are looking into ways of achieving this, by incorporating information from other sequences such as DCE.Acknowledgements
No acknowledgement found.References
1. Panagiotaki E, Walker-Samuel S, Siow B, Johnson SP, Rajkumar V, Pedley RB, et al. Noninvasive quantification of solid tumor microstructure using VERDICT MRI. Cancer Res. 2014;74:1902–12. doi: 10.1158/0008-5472.CAN-13-2511.
2. Panagiotaki E, Chan RW, Dikaios N, Ahmed HU, O'Callaghan J, Freeman A, et al. Microstructural characterization of normal and malignant human prostate tissue with vascular, extracellular, and restricted diffusion for cytometry in tumours magnetic resonance imaging. Investigative radiology 2015; 50(4): 218-27.
3. Roberts TA, Hyare H, Agliardi G, Hipwell B, d'Esposito A, Ianus A, et al. Quantitation of brain tumour microstructure response to Temozolomide therapy using non-invasive VERDICT MRI. bioRxiv 182675
4. Panagiotaki E, Schneider T, Siow B, Hall MG, Lythgoe MF, Alexander DC. Compartment models of the diffusion MR signal in brain white matter: A taxonomy and comparison. NeuroImage. 2012;59:2241–2254.
5. Zhang H, Schneider T, Wheeler-Kingshott CA, Alexander DC. NODDI: Practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage. 2012; 61(4):1000–16.
Figures