2682
Relationship Between Gray Matter Volume Reductions and TPH1 Polymorphisms in Depressive Disorder Patients with Suicidal AttemptsGeon-Ho Jahng1, Jin Kyung Park2, Seong Jong Yun1, Chang-Woo Ryu1, Wook Jin1, and Dal Mo Yang1
1Radiology, Kyung Hee University Hospital at Gangdong, Seoul, Korea, Republic of, 2Psychiatry, Kyung Hee University Hospital at Gangdong, Seoul, Korea, Republic of
Synopsis
To investigate relationship between gray matter volume (GMV) changes and TPH1 polymorphisms in depressive disorder (DD) patients with suicidal attempts (SA), 13 DD-SA patients and 20 healthy controls were scanned three-dimensional (3D) T1-weighted image to obtain GMV in the brain. In addition, TPH1 rs1800532 and rs1799913 polymorphisms were obtained. The patients showed significant GMV reduction. The right precentral and postcentral gyri GMV values of AA and CA genotypes patients were significantly decreased compared to those of CC genotype subjects, indicating that both GMV reductions and TPH1 A allele may be involved in the pathogenesis of DD-SA patients.
Introduction
Recently, many neuroimaging studies using MRI have elucidated that structural changes of brain areas have been reported in depressive disorder and suicidal behavior (SB), in which TPH1 also has been known as a promising candidate gene. Sixty percent of people who committed suicide had a history of depressive disorder (1). Previous studies investigating SB in depressive disorder patients reported local gray matter changes of several cortical and subcortical structures (2,3, 4, 5). This growing evidence shows that genetic factors are involved in the pathophysiology both of depressive disorder and SB. The objective of this study was to investigate the relationship between gray matter volume (GMV) changes and tryptophan hydroxylase 1 (TPH1) rs1800532 and rs1799913 polymorphisms (6), previously found to be associated with depressive disorder and SB.Methods
Thirteen (12 females and 1 male; mean age= 31.9±10.0 years; age range= 20–47 years) depressive disorder patients with suicidal attempts (SA) and twenty (13 females and 7 males; mean age=33.6±6.2 years; age range= 22–48 years) healthy controls were scanned to obtain GMV using a 3D-T1-weighted imaging sequence with a 3T MRI. Statistical Parametric Mapping 12 (SPM12) software was used to process images and to perform voxel-based analysis. SNP genotyping was conducted using direct sequencing using the primers for both rs1800532 and rs1799913. In order to investigate the relationship between GMV changes and alleles, differences of GMV values according to genotypes (minor allele homozygotes and heterozygotes vs. major allele homozygotes; minor allele homozygotes vs. heterozygotes and major allele homozygotes) were compared using an independent samples t-test.Results
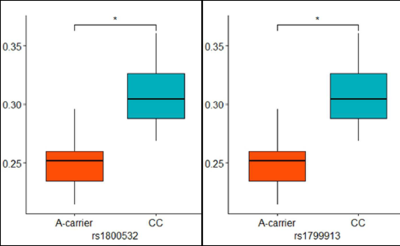
First, a correlation was found between BIS-11 scores and the ROI 3 GMV values (r = 0.647, p =0.017) in the patients. Second, the patients showed significant GMV reduction in left cerebral region including middle frontal gyrus, inferior frontal gyrus, and anterior cingulate cortex; in right middle temporal gyrus; in left cerebellar tonsil; and in right cerebral region including precentral gyrus and postcentral gyrus (corrected p < 0.005). Third, the right precentral and postcentral gyri GMV values of AA and CA genotypes patients were significantly decreased compared to those of CC genotype subjects (corrected p = 0.040).Discussion
This is a study attempting to elucidate neurobiological mechanisms underlying depressive disorder with SB by investigating a link between GMV changes and genetic polymorphisms. The patients showed significant GMV reductions in the left cerebral region including middle frontal gyrus (BA 10), inferior frontal gyrus, and anterior cingulate cortex (BA 32). GMV reductions in the middle frontal gyrus are consistent with previous studies with depressive disorder patients. Abnormalities in activity of the middle frontal gyrus were reported in functional studies of depression. Altered functional connectivity between the middle frontal gyrus and other regions such as insula and anterior cingulate cortex was also found in depression. Taken together, changes in the middle frontal gyrus GMV could be essential to the pathophysiology of depression, particularly to emotional processing.Conclusion
GMV was decreased in depressive disorder patients with SA in several regions of frontal lobe, temporal lobe, paracentral gyrus, and cerebellum The paracentral gyrus GMV reduction was associated with A carriers of rs1800532/rs1799913 in the patients. These results suggest that GMV changes and TPH1 polymorphisms may be simultaneously implicated in the pathogenesis of depression with SB.