2583
Arteriovenous Structure and Blood Flow Abnormalities in Parkinson’s Disease1Department of MRI, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2Wayne State University, Detroit, MI, United States, 3Department of Neurology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 4Magnetic Resonance Innovation INC, Detroit, MI, United States
Synopsis
Few researchers have paid attention to the vascular supply and venous outflow in Parkinson’s disease (PD). In this work, we evaluated arterial inflow and venous outflow and looked for the presence of abnormal venous structure. We found that there was a significant correlation of reduced arterial flow with reduced internal jugular vein (IJV) flow. We also found there were a large number of PD patients with no or little flow in the left IJV compared to healthy control group. These results suggest that abnormal flow could be one factor in the development of or progression of PD in some patients.
Introduction
The cause of Parkinson's disease (PD) is still unknown. Early diagnosis of PD has always been a clinical challenge and is critical for better treatment and improvement of quality of life. At present, routine magnetic resonance imaging (MRI) does not provide enough information to improve the early diagnosis of PD. Reduced flow into the brain or increased outflow from the brain may serve as a biomarker for PD. Therefore, our goal is to compare the presence of vascular abnormalities on both the arterial and venous sides with the presence of white matter hyperintensities (WMH) and clinical scores such as the UPDRS (Unified Parkinson Disease Rating Scale) and HY (Hoehn and Yahr) scales.Methods
A total of 80 PD patients and 55 age and sex-matched healthy controls (HC) were included in the study. Patients were aged 59.6+/-9.2 years with 45 females while controls were aged 57.5+/-9.0 years with 28 females. The disease duration for the PD subjects was 3.4+/-3.0 years. The UPDRS score ranged from 14-101 with a median UPDRS score of 38. Participants were imaged once on one of two 3T Siemens Prisma scanners (Erlangen, Germany). The MRI protocol included: T1 MP-RAGE (Magnetization Prepared Rapid Acquisition Gradient Echo), 2D time-of-flight MR venography, 2D FLAIR (Fluid Attenuated Inversion Recovery) and 2D FQ (Flow Quantification) among other sequences. Images were processed using SPIN software (SpinTech Inc., Bingham Farms, MI) (Figure 1). Regions of interest (ROI) were drawn on the white matter lesions in the T2W FLAIR images. The PD patients and HC were divided into four categories as described in Liu et al1 based on MRV and flow findings. In short, category 1 shows absence of the left IJV; category 2 shows very low flow in the left IJV; category 3 shows some flow but still abnormally low in the left IJV and category 4 shows normal vessels and normal flow (Figure 2). A WMH cutoff of 1cc was used to separate high WMH hyperintensity subjects from more normal appearing white matter.2 Further, an outflow of 7ml/s was used as a biomarker for abnormally slow flow in the total IJV flow.3Results
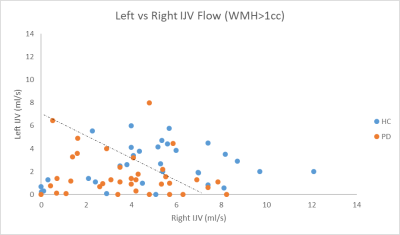
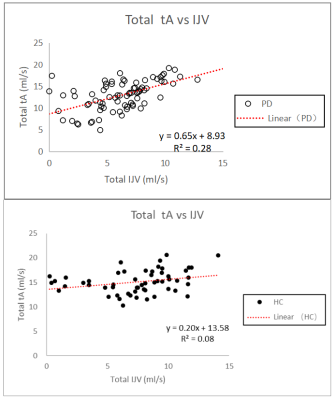
The main findings in this work relate to abnormal flow characteristics in both the arterial and venous systems for PD patients. There were four significant findings. First, we found that total arterial (tA) flow showed a significant difference between HC and PD. The average tA was 15.1ml/s +/- 2.3 ml/s for HC and 13.0ml/s +/- 3.4 ml/s for PD patients (p < 0.001). Using a cutoff of two standard deviations below the mean tA (10.5 ml/s), only 2% of the HC group fell below this lower limit while 24% of the PD group fell below this value (Figure 3). Second, keeping only those cases with WMH volumes greater than 1 cc and using a cutoff of 7 ml/s for total IJV, 34% of the HC group fell below 7 ml/s while 72% of the PD group fell below this value (Figure 4). Third, tA correlated with tIJV for PD patients (R² = 0.28) but not for HC (R² = 0.08). For the PD cases, the relationship was tA=0.65tIJV+8.93 (Figure 5). Fourth, the PD patients showed a total of 29 cases (41%) in categories 1 and 2 while the HC showed only 7 (13%).Discussion
The abnormally low flow seen in the IJVs is similar to that reported for MS patients4. For the PD group, there were many more cases with abnormal venous vasculature and function (categories 1 and 2) than the HC group. A new finding in this work is that the tA flow also decreased well below normal levels which has not been seen in MS studies and has not previously been reported in PD studies. Given the long time it takes to develop PD, one might ask what is the role of chronically reduced blood flow into and out of the brain? Finally, an interesting future study would be to compare the increases in iron content seen in the substantia nigra with the reduced flows reported in this work.Conclusion
This study found abnormalities in the arteriovenous structure and blood flow in PD patients using a high resolution 2D FQ sequence. Specifically, there was a high proportion of PD patients with abnormal left IJV structure; a tA value less than 10.5ml/s; and a preponderance of PD patients who exhibited tIJV blood flow values < 7ml/s compared to HC subjects. These three imaging indicators may serve as early biomarkers for PD and may open a new door for studying the etiology of PD.Acknowledgements
No acknowledgement found.References
1. Liu M, Xu H, Wang Y, et al. Patterns of chronic venous insufficiency in the dural sinuses and extracranial draining veins and their relationship with white matter hyperintensities for patients with Parkinson's disease. Journal of Vascular Surgery, 2015, 61(6):1511-1520.
2. Raz N, Yang Y, Dahle C L, et al. Volume of white matter hyperintensities in healthy adults: contribution of age, vascular risk factors, and inflammation-related genetic variants. BBA - Molecular Basis of Disease, 2012, 1822(3):361-369.
3. Haacke EM, Sethi SK, Jiang J, et al. The role of magnetic resonance imaging in assessing venous vascular abnormalities in the head and neck: a demonstration of cerebrospinal venous insufficiency in a subset of multiple sclerosis patients. Veins and Lymphatics 2015; volume 4:5012.
4. Sethi S K, Utriainen D T, Daugherty A M, et al. Jugular Venous Flow Abnormalities in Multiple Sclerosis Patients Compared to Normal Controls. Journal of Neuroimaging, 2015, 25(4):600-607.
Figures