2144
Usefulness of Left Ventricular Flow Component Analysis in Patients with Bicuspid Aortic Valve Disease InsufficiencyJulio Garcia1, Alireza Sojoudi2, An Le2, Michael S Bristow1, Carmen Lydell1, Andrew G Howarth1, Paul W Fedak1, and James White1
1University of Calgary, Calgary, AB, Canada, 2Circle Cardiovascular Imaging Inc., Calgary, AB, Canada
Synopsis
Acute aortic insufficiency (AI) is often developed in patients with bicuspid aortic valve (BAV). Flow component analysis (FCA) derived from 4D flow MRI can be used as a novel marker of LV function worsening. This study aimed to explore the value of FCA in the assessment of AI severity in BAV patients.
BACKGROUND
Acute aortic insufficiency (AI) is often developed in patients with bicuspid aortic valve (BAV). The acute volume overload in the left ventricle (LV) usually results in severe pulmonary congestion as well as a low forward cardiac output. 4D flow MRI allows for non-invasive assessment of 3D intracardiac flow. Flow component analysis (FCA) derived from 4D flow MRI has emerged as a novel marker of LV function worsening. This study aimed to explore the value of FCA in the assessment of AI severity in BAV patients.METHODS
39 subjects (30 BAV, age 44±13 years, 10 women; 9 healthy controls, age 27±12 years, 5 women) were prospectively enrolled and completed a standardized MRI protocol at 3T inclusive of 4D Flow. Patients with mitral insufficiency were excluded. AI severity was graded using regurgitant fraction as mild, moderate, and severe according to AHA guidelines. 4D flow MRI was analyzed using a commercial software (Circle Cardiovascular Imaging Inc., Calgary, Canada) (Fig. 1A). The LV was segmented and used to generated pathlines along the cardiac cycle (Fig. 1B). The pathlines were considered to represent the whole intraventricular blood volume. Blood volume was dived into four functional components: 1) direct flow (DirF) that enters the LV during diastole and leaves the LV during systole; 2) retained flow (RetF) that enters the LV during diastole but does not leave during systole; 3) delayed ejection (DelE) flow that resides inside the LV during diastole and leaves during systole; 4) Residual volume (ResV) that resides with in the LV. Flow analysis planes prescribed in the aortic valve (AoV) and mitral valve (MV) to quantify peak velocity (PV), net flow (NF), retrograde flow (RF) and regurgitant fraction (RFF) (Fig. 1B).RESULTS
BAV subjects showed no significant elevation in PV and NF versus healthy controls (p>0.05). RFF was elevated in BAV patients (1±1 % vs. 9±10 %, p=0.018) consistent with valvular insufficiency (n=14, including all AI grades). FCA showed significant differences between controls (Fig. 1C) and BAV in DirF (p=0.029) and ResV (p=0.045) (Fig. 1D); and in controls versus BAV-AI in DirF (p=0.009) and DelE (p=0.033) (Fig. 1E).CONCLUSION
In patients with BAV valve disease FCA derived from 4D flow MRI identifies significant intraventricular hemodynamic differences between controls and BAV, and controls versus BAV with AI. AI significantly impact was observer in DirF and DelE, as indicator of LV worsening. Future investigation is warranted to explore how FCA novel markers of LV hemodynamics of AI progression in valve disease.Acknowledgements
Mitac IT07679 and IT07680References
No reference found.Figures
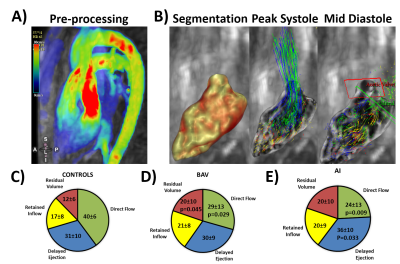
Figure 1. Flow component analysis
(FCA). Panel A shows the preprocessing of 4D flow MRI data which included
air-filing, removal of static tissue, eddy-current correction, and
phase-unwrapping. Panel B shows the segmentation of left ventricle using region
growing, the quantification of pathlines
over the cardiac cycle. Examples of pathlines
at peak systole and mid diastole are presented. Panel C summarize FCA for
controls. Panel D summarize FCA for bicuspid valves (BAV). Panel E summarize
FCA for BAV with acute aortic insufficiency (AI).