2005
T1 is significantly higher in myocardial T1 when measured during free breathing than at inspiration1Academic Radiology, University of Sheffield, Sheffield, United Kingdom
Synopsis
Release of breath hold results in misalignment of the myocardium during cardiac T1 mapping. Several registration methods have been developed to overcome this [1][2][3], however, it has not been established whether the process of respiration effects myocardial T1 when mapped with dynamic MOLLI sequences. 10 healthy volunteers underwent 1.5T MOLLI T1 mapping during both breath hold and free breathing acquisition. Images were registered using synthetic images created via a combined inversion recovery and respiratory signal modulation model, which was verified using Dice Similarity Coefficient. Myocardial T1 was found to be higher in healthy volunteers when acquired during free breathing, when compared to inspiration.
Background
For patients with cardiac or pulmonary disease, breath holds can be difficult or unachievable. Release of breath hold will result in misalignment of the myocardium during cardiac T1 mapping. Several registration methods have been developed to overcome this, however, it has not been established whether the process of respiration affects the measured myocardial T1.Purpose
To present a method of image registration and T1 mapping for free-breathing MOLLI images and evaluate whether free breathing images show significantly different T1 when compared to breath hold myocardial T1.Methods
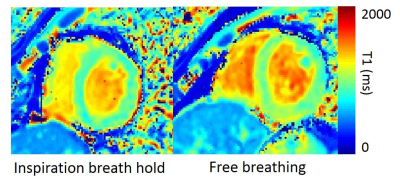
Free breathing images were registered using synthetic images which are created using a combined inversion recovery and respiratory signal-modulation model, which describes the signal intensity of a group of pixels over time as the combination of inversion recovery and respiratory motion, see Figure 1. The model uses signal intensity from a group of pixels within the images to determine respiratory rate. Respiratory rate is then used to select images from the same respiratory state from which to create a set of spatially aligned synthetic images. Myocardial and blood T1 values were calculated using two methods: 1) drawing regions of interest on the myocardial septum on each image, and calculating T1 from the mean signal of each region, and 2) drawing regions of interest onto registered T1 maps in the myocardial septum. T1s calculated using each method were compared for consistency. Myocardial alignment was determined by segmenting the left ventricle and calculating Dice Similarity Coefficient for each set of images before and after registration. 10 healthy volunteers underwent MOLLI T1 mapping acquisitions at 1.5T in both inspiration breath hold and during free breathing. T1 mapping was performed using a 2D 3-3-5 MOLLI sequence in a single short axis slice. Flip angle: 35◦; image dimensions: 128x128; TR: 3.20ms; TE: 1.41ms; parallel imaging using sensitivity encoding with acceleration factor 2; FOV: 400mm; slice thickness: 5.1mm.Results
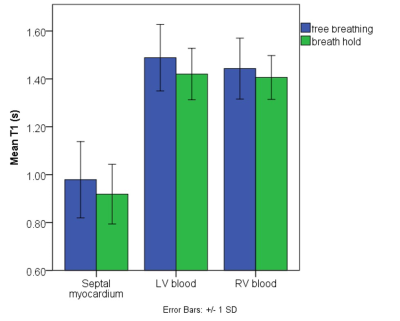
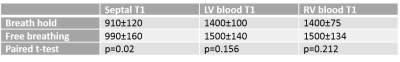
DSC was significantly increased after image registration, p<0.001, see Figure 2 and Table 1. DSC was improved in all patients, with an unregistered DSC range of 0.55-0.75 and a registered DSC range of 0.60-0.78. There were no significant differences between myocardial septal T1 values measured from T1 maps when compared to myocardial septal T1 values measured from mean signal calculated from individual regions of interest drawn on MOLLI images (p=0.903). In breath hold, myocardial septal T1 = 910±120ms was significantly lower than in free breathing T1 = 990±160ms (p=0.002). Blood T1 was not significantly higher during free breathing.Discussion and conclusion
Myocardial alignment was significantly increased due to image registration, and resulted in myocardial T1 values consistent with those determined from mean signal from ROIs drawn on each image. This indicates that the registration and respiratory model did not lead to erroneous T1 values. Myocardial T1 was found to be significantly higher during free breathing. The predominant limitation of this method is that it does not compensate for out-of-plane motion. It is likely that the imaging plane will include images where some of the protons from another imaging plane with a different magnetization history, including non-inverted protons. However, the mixing of non-inverted spins into the imaging plane, would be expected to shorten resultant T1, and our findings are that free-breathing acquisition resulted in a longer T1. It is not clear what the mechanism of the observed increase in T1 during respiration is, however, it is known that myocardial perfusion and oxygenation change with breathing manoeuvres and this may be the cause of the differences seen in myocardial T1.Acknowledgements
No acknowledgement found.References
[1] H. Xue, S. et al., (2012). “Motion correction for myocardial T1 mapping using image registration with synthetic image estimation,” Magnetic Resonance in Medicine, 67:644-655
[2] H. Xue, et al., (2013). “Phase-sensitive inversion recovery for myocardial t1 mapping with motion correction and parametric fitting,” Magnetic Resonance in Medicine, 69:1408–20
[3] Q. Tao, et al., (2018)“Robust motion correction for myocardial t1 and extracellular volume mapping by principle component analysis-based groupwise image registration,”, Journal of Magnetic Resonance Imaging, 47:1397–1405
Figures