1976
Velocity transfer function in the right pulmonary artery correlates with right ventricular remodeling and pulmonary functional impairments in COPD1Medicine, University of Alabama at Birmingham, Birmingham, AL, United States, 2Auburn University, Auburn, AL, United States, 3Valley Medical Group, Paramus, NJ, United States
Synopsis
Chronic
obstructive pulmonary disease (COPD) is often associated with pulmonary artery (PA)
hypertension (PH), however a mild to moderate PH is frequently not identified
on non-invasive testing in COPD patients. The novel non-invasive cardiovascular
magnetic resonance (CMR) derived parameter, velocity transfer function (VTF), has
been recently shown to correlate with invasive PA impedance. Here, we tested the
VTF to evaluate its association with clinical/pulmonary functional indices and
RV remodeling in patients in early COPD. We found that elevated VTF mean high
frequency modulus was associated with major clinical and functional criteria
indicating cardiovascular/respiratory dysfunction, which may link to PH.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death in the United States.(1) Pulmonary artery (PA) hypertension (PH) provides important prognostic information in COPD, however the majority of patients with COPD have a mild to moderate PH that is frequently not identified on non-invasive testing.(2) Recently, we have validated a novel non-invasive cardiovascular magnetic resonance (CMR) derived parameter that reflects pulsatile and resistive properties of the PA.(3) This novel parameter relies on the fact that the compliant PA walls cause frequency-dependent changes in the input velocity profile as it travels through the artery thereby producing the output velocity profile. The frequency-dependent relationship between the input and output velocity profiles was described by a velocity transfer function (VTF), which is the relationship between the frequency spectra of input and output velocity.(3) In patients with suspected and invasively proven PH, we have found that VTF correlates with invasive PA impedance, pulmonary vascular resistance (PVR), and right ventricular (RV) remodeling.(3) Moreover, the mean high frequency modulus (MHFM) of VTF >1 accurately predicted an increased PVR.(3) Increased PA stiffness represents the earliest physiological manifestation of PA remodeling that can result in increased PVR and RV afterload, and eventually pulmonary vascular disease, including PH and COPD.(4-6) We hypothesize that increased PA stiffness in early COPD stages can be identified by VTF by the presence of elevated MHFM. Therefore, we tested VTF to evaluate its association with clinical/pulmonary functional indices and RV remodeling in patient in the early COPD stages.METHODS
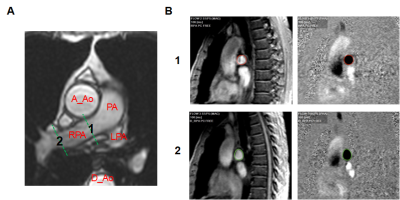
We prospectively recruited 21 patients (60±9 years, of both sex) with history of pulmonary/lung disease, at different stages of COPD. As CMR study requires a prolonged laying supine, on the back, the patients with severe airflow limitation (i.e., later stages COPD) were not enrolled. This study was approved by the UAB Institutional Review Board and all participants gave written informed consent. Patients completed questionnaires regarding symptoms and underwent spirometry and 6-minute-walk test (6MWT). CMR was performed on a 1.5-T magnetic resonance scanner (GE Signa, Milwaukee, Wisconsin) optimized for cardiac application. Phase-contrast CMR technique was used for flow measurements in the right PA (RPA) as described (Figure 1).(3) Phase-contrast CMR was performed using ECG gated, breath-hold fast gradient recalled echo phase-contrast sequence as previously described.(3) Contours were drawn and mean velocity-time profiles over a cardiac cycle were computed using CAAS MR Flow 1.2 (Pie Medical Imaging, Netherland) and exported to MATLAB 2015a for VTF and MHFM computation (Figure 2).(3) RV and LV systolic function and remodeling were assessed by cine-CMRI. ECG-gated breath-hold steady-state free-precision technique was used to obtain standard 2-chamber, 4-chamber and short-axis views with parameters and analysis previously described.(7, 8) Clinical/pulmonary functional indices and LV and RV function was compared in patients with MHFM<1 (low MHFM) vs. those with MHFM>1 (high MHFM).(3)RESULTS
VTF and VTF MHFM in groups are shown in Figure 3. Patients with high VTF MHFM (n=9) demonstrated a trend towards worsening in different COPD evaluation/prognostic systems, including Modified Medical Research Council Dyspnea Scale (mMRC)(9) (Figure 4A), BODE(10) (Body mass index, airflow Obstruction, Dyspnea and Exercise capacity) index (Figure 4B), and GOLD(11) (Global Initiative for Obstructive Lung Disease) grading system (Figure 4C) than those with low MHFM (n=12), but the difference did not reach statistical significance. However, high MHFM group had significantly lower performance during 6MWT (Figure 4D). High MHFM group also had worse lung function tests expressed either as absolute values of forced expiratory volume in 1 sec (FEV1) and vital capacity (FVC) or expressed as percent of predicted values (Figure 4E and 4F, respectively). There was no difference between groups in the LV mass, LV and RV ejection fraction and ventricular volumes. However, the high MHFM group had a larger absolute RV mass (Figure 4G) or indexed by the height^2.7 (p=0.07), and more concentric right ventricle assessed as RV mass/volume ratio (Figure 4H).DISCUSSION
Despite a limited patient number in our study, high VTF MHFM was consistently associated with major clinical and functional criteria indicating cardiovascular and respiratory dysfunction. Our results support our hypothesis that the VTF MHFM can serve as non-invasive surrogate for PA impedance and identify increased PVR, which can lead to PH hypertension. More research is needed in a larger patient cohort for accurate evaluation of the VTF MHFM application in COPD.CONCLUSION
The non-invasive VTF MHFM reflects changes suggestive of increased PA stiffness and PVR in COPD patients. VTF can be utilized during a CMR study in addition to routine assessment of RV and pulmonary vascular function.Acknowledgements
No acknowledgement found.References
1. Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, et al. The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA. 2018;319(14):1444-72.
2. Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective. Chest. 2010;137(6 Suppl):39S-51S.
3. Gupta A, Sharifov OF, Lloyd SG, Tallaj JA, Aban I, Dell'Italia LJ, et al. Novel Non-Invasive Assessment of Pulmonary Arterial Stiffness Using Velocity Transfer Function. J Am Heart Assoc. 2018;7:e009459.
4. Thenappan T, Prins KW, Pritzker MR, Scandurra J, Volmers K, Weir EK. The Critical Role of Pulmonary Arterial Compliance in Pulmonary Hypertension. Ann Am Thorac Soc. 2016;13(2):276-84.
5. Weir-McCall JR, Struthers AD, Lipworth BJ, Houston JG. The role of pulmonary arterial stiffness in COPD. Respir Med. 2015;109(11):1381-90. 6. Stevens GR, Garcia-Alvarez A, Sahni S, Garcia MJ, Fuster V, Sanz J. RV dysfunction in pulmonary hypertension is independently related to pulmonary artery stiffness. JACC Cardiovascular imaging. 2012;5(4):378-87.
7. Wells JM, Iyer AS, Rahaghi FN, Bhatt SP, Gupta H, Denney TS, et al. Pulmonary artery enlargement is associated with right ventricular dysfunction and loss of blood volume in small pulmonary vessels in chronic obstructive pulmonary disease. Circulation Cardiovascular imaging. 2015;8(4).
8. Feng W, Nagaraj H, Gupta H, Lloyd SG, Aban I, Perry GJ, et al. A dual propagation contours technique for semi-automated assessment of systolic and diastolic cardiac function by CMR. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2009;11:30.
9. Society AT. Surveillance for respiratory hazards in the occupational setting: ATS statement. Am Rev Respir Dis. 1982;126(5):952-6.
10. Puhan MA, Garcia-Aymerich J, Frey M, ter Riet G, Anto JM, Agusti AG, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet. 2009;374(9691):704-11.
11. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. American journal of respiratory and critical care medicine. 2007;176(6):532-55.
Figures