1694
Detection of Portal Vein Thrombosis in Patients with Hepatocellular Carcinoma: Can Gadoxetic Acid–enhanced MR Imaging Replace CT?1Seoul National University Hospital, Seoul, Korea, Republic of
Synopsis
Gadoxetic acid-enhanced magnetic resonance imaging (GA-MRI) provides higher sensitivity for the detection of HCCs than CT or MRI using extracellular contrast media, but may have a disadvantage in detection of portal vein thrombosis (PVT) related with decreased contrast between the portal vein and liver parenchyma during dynamic phase. For detection of PVT in patients with HCC, we demonstrated that GA-MRI was noninferior to CT for sensitivity (78.8% versus 77.7%, respectively) and was superior to CT for specificity (95.4% versus 92.4%, respectively). For characterization of the PVT as benign or malignant, the GA-MRI showed noninferior accuracy to CT (93.7% versus 92.4%).
INTRODUCTION
Hepatocellular carcinoma (HCC) in patients with liver cirrhosis is a common cause of malignant or bland portal vein thrombosis (PVT). Malignant PVT is an indicator of poor prognosis, while bland PVT can be resolved by anticoagulation and/or thrombolytic treatment 1,2. Hence, the detection of PVT and differentiation of malignant from bland PVT is important. Gadoxetic acid-enhanced magnetic resonance imaging (GA-MRI) provided higher sensitivity for the detection of HCCs than CT or MRI using extracellular contrast media, due to the improved lesion-to-liver contrast during the hepatobiliary phase imaging 3, 4. However, GA-MRI may have a potential disadvantage in detection of PVT related with the decreased contrast between the portal vein and liver parenchyma during dynamic phase, because of early uptake of gadoxetic acid which starts approximately 1 minute after administration of the contrast agent 5. Previous studies demonstrated that CT showed a moderate sensitivity ranged from 68% to 86%, in terms of evaluation of PVT, and gadoxetic acid-enhanced MR imaging (GA-MRI) has a sensitivity of 70—84% 6,7. However, there have been no study which directly compared diagnostic performance of CE-GA-MRI and CT for detection and characterization of PVT yet. Therefore, the purpose of our study was to compare the diagnostic performance of GA-MRI and CT in the detection and characterization of PVT in patients with HCC.METHODS
In this retrospective study, we included 524 patients (411 men and 113 women; mean age, 57.0 ± 10.1 years) with HCC who underwent the GA-MRI and CT between January 2007 and May 2017. There were patients with malignant PVT (n=178) or benign PVT (n=84), and age- and sex- matched patients without PVT (n=262). Two radiologists independently reviewed the GA-MRI and CT images and assessed the sensitivity and specificity for the detection of PVT and accuracy in the characterization of PVT. The presence of PVT was assessed using the Liver Imaging Reporting and Data System. Statistical analysis was performed by using generalized estimating equation and noninferiority test.RESULTS
Diagnostic Performance of GA-MRI for PVT
The pooled sensitivity for detection of PVT for GA-MRI was noninferior to that for CT (78.8% [413/524] versus 77.7% [407/524], respectively) with a difference of 1.1% (95% CI; -1.7, 4.0) (P=.440). The pooled specificity for detection of PVT for GA-MRI was superior to that for CT (95.4% [500/524] versus 92.4% [484/524], respectively) with a difference of 3.0% (95% CI; 1.1, 5.0) (P=.002). For characterization of the PVT as benign or malignant, the GA-MRI showed noninferior accuracy to CT (93.7% [387/413] versus 92.4% [376/407]) with a difference of 1.3% (95% CI; -1.6, 4.3) (P=.385). The interobserver agreement of the GA-MRI was higher than that of the CT (κ=0.827 vs. 0.762)
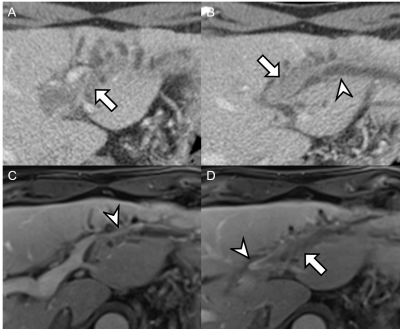
Imaging Findings of malignant PVT
In the malignant PVT group, vessel expansion and continuity of the tumor was more frequent on GA-MRI than on CT (88.8% [316 of 356 patients] versus 82.0% [292 of 356 [patients] for vessel expansion and 93.3% [332 of 356 patients] versus 87.4% [311 of 356 patients] for continuity of the tumor, respectively) (P=.002 and .001, respectively). In the benign PVT group, however, there was no imaging feature that showed significant difference between the GA-MRI and CT.
The high signal intensity on T2-weighted imaging and diffusion restriction are unique to the GA-MRI imaging. Owing to these two imaging features, in the malignant PVT group, the GA-MRI additionally revealed PVTs in 25 patients in whom CT demonstrated no PVT. Furthermore, 12 patients whose PVTs were considered as benign or indeterminate on CT were correctly classified into the malignant PVTs on the GA-MRI.
DISCUSSION
We demonstrated that the diagnostic performance of the GA-MRI for detection of PVT in patients with HCC was comparable to that of the CT. This good performance of the GA-MRI for detection of PVT may be attributed to the multiple parameters exploited in the MR. In addition to the dynamic contrast-enhanced imaging, diffusion- and T2- weighted imaging are performed in the GA-MRI. In our study, these two parameters aided detection and characterization of the malignant PVT in 37 patients on the GA-MRI which were not detected or were considered not malignant on the CT. Therefore, the theoretical disadvantage of the GA-MRI for detection of PVT, if existed, may have been overcame by the additional parameters unique to the GA-MRI compared to the CT.
CONCLUSION
For detection of PVT in patients with HCC, GA-MRI was noninferior to CT for sensitivity and was superior to CT for specificity. GA-MRI was noninferior to CT regarding accuracy for characterization of PVT as well.Acknowledgements
Institutional review board approved this retrospective study and informed consent was waived.
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding.
The authors appreciate the Medical Research Collaborating Center at Seoul National University Hospital for statistical analysis and consultation.
References
1. Shah SA, Greig PD, Gallinger S, et al. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg 2006;202(2):275-283.
2. Qian LJ, Zhu J, Zhuang ZG, S, et al. Differentiation of neoplastic from bland macroscopic portal vein thrombi using dual-energy spectral CT imaging: a pilot study. Eur Radiol 2012;22(10):2178-2185.
3. Kitao A, Zen Y, Matsui O, et al. Hepatocellular carcinoma: signal intensity at gadoxetic acid-enhanced MR Imaging--correlation with molecular transporters and histopathologic features. Radiology 2010;256(3):817-826.
4. Lee YJ, Lee JM, Lee JS, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology 2015;275(1):97-109.
5. Rohrer M, Bauer H, Mintorovitch J, et al. Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol 2005;40(11):715-724.
6. Rossi S, Ghittoni G, Ravetta V, et al. Contrast-enhanced ultrasonography and spiral computed tomography in the detection and characterization of portal vein thrombosis complicating hepatocellular carcinoma. Eur Radiol 2008;18(8):1749-1756.7. Kim JH, Lee JM, Yoon JH, et al. Portal Vein Thrombosis in Patients with Hepatocellular Carcinoma: Diagnostic Accuracy of Gadoxetic Acid-enhanced MR Imaging. Radiology 2016;279(3):773-783.
Figures