1077
Studying human placental function ex-vivo using perfusion methods in MRI1Sagol Brain Institute, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel, 2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel, 3Sagol School of Neuroscience, Tel Aviv University, Tel Aviv, Israel, 4Pediatric Radiology, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel, 5Pediatric Neurology, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel, 6Obstetrics and Gynecology, Lis Maternity Hospital, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel, 7Department of Medical Engineering, Tel Aviv Academic College of Engineering, Tel Aviv, Tel Aviv, Israel
Synopsis
The aim of this study was to investigate the functional characteristics of the human placenta ex-vivo using a novel MR compatible perfusion system. Fifteen normal human placentas were scanned ex-vivo; bolus arrival time (BAT) and flow were extracted from TWIST data. Higher BAT and lower flow values were found in placentas with peripheral cord insertion. Significant correlations were obtained between BAT and the linear distance of the blood vessel from cord insertion location. This is the first work that studied the perfusion of human placentas with MRI and provides information regarding the relation between placental structure and function.
Abstract
INTRODUCTION
Normal placental development and function are vitally important for healthy pregnancy and normal fetal development (1-6). There is strong evidence that many of the major complications of pregnancy have their roots in placental insufficiency. To date, the gold standard for in-vivo diagnosis of placental function is US Doppler, which gives only an indirect assessment. Several studies investigated human placental structure and function ex-vivo (7), yet understanding regarding human placental function and its association with its structure, pregnancy risks and outcomes is limited. The aim of this study was to investigate the functional characteristics of the normal human placenta ex-vivo using a novel MR compatible perfusion system and advanced MR methods implemented from the field of neuro-imaging.
METHODS
Placentas and MR protocol Fifteen normal placentas were obtained from donors who provided informed consent after full term pregnancies (38-41 weeks’ gestation), up to one hour after delivery of healthy newborns weighing between 2700 kg to 3900 kg. Placentas were rinsed with a solution of saline and heparin before being connected to an MR compatible perfusion system for ex-vivo imaging of human placenta, that mimics the pulsatile flow of the fetal cardiovascular system (Fig. 1). Dynamic time-resolved 3D magnetic resonance angiography (MRA) technique with Interleaved Stochastic Trajectories (TWIST) with high temporal (0.84 sec) and spatial resolution (0.937X0.937X1 mm) was used to capture the multiple arterial, mixed, venous phase images during the passage of a contrast agent through the vascular anatomy. A mixture of 3 ml water and 0.3 ml of contrast agent (Gadolinum Dotarem 0.5M) was injected through an access in the inflowing pipe to the placental arteries, 10-20 sec after the scan began. Image Analysis Image analysis was performed using Matlab, and included: Bolus arrival time (BAT) and flow calculation. The algorithm consisted of the following steps: (1) Data normalization according to baseline; (2) Threshold vascular tree segmentation by angiography mask creation; (3) Bolus arrival time (BAT) calculation and BAT maps creation; (4) Flow maps creation by Gaussian fitting to the intensity over time and dividing the area under curve by the full width in half maximum; (5) Normalized BAT and flow histograms were extracted for each placenta. Placental function was studied in relation to cord insertion location (distance from center in percentages), while referring to para-central cord insertion (cord insertion is more than 3cm from placental edges) vs. marginal/peripheral (cord insertion is less than 3cm from placental edges).
RESULTS
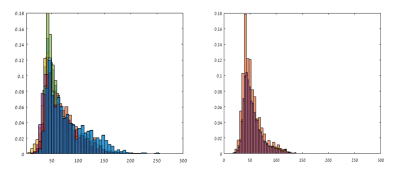
All 15 placentas were successfully perfused, scanned, and analyzed providing BAT and flow maps. Fig. 2 shows coronal minimum intensity projection (MIP) of the BAT map (A,B), and flow (C, D) of typical placentas one (A, C) with central cord insertion and one (B, D) with peripheral cord insertion. Significant correlations (mean r=0.81 p<0.01) were obtained within each placenta between BAT values and the distance of the blood vessel from cord insertion location. Higher values of BAT were obtained in placentas with peripheral (marginal) cord insertion compared to placentas with para-central cord insertion. This can be seen in the histogram of the values of BAT in the two groups of placentas (Fig. 3). Lower values of flow were obtained in placentas with peripheral (marginal) cord insertion compared to placentas with para-central cord insertion. This can be seen in the histogram of the values of flow in the two groups of placentas (Fig. 4).
SUMMARY
-This is the first study to investigate ex-vivo perfusion of the human placenta using MR compatible perfusion system.
-This study demonstrates the ability to quantitatively characterize flow pattern of the entire vascular tree of ex-vivo placentas post-partum.
-Preliminary results suggest significant differences in perfusion between normal placentas with para-central vs. peripheral cord insertion.
-Our current efforts are to study the correlation between placental function and structure, and to investigate conditions of placental insufficiency.
Acknowledgements
We thank the mothers for their agreement to use the placentas for research. We are grateful to Uri Zaretzky for building the perfusion systemReferences
1. Arck, P.C. and K. Hecher, Fetomaternal immune cross-talk and its consequences for maternal and offspring's health. Nat Med, 2013. 19(5): p. 548-56.
2. Evain-Brion, D. and A. Malassine, Human placenta as an endocrine organ. Growth Horm IGF Res, 2003. 13 Suppl A: p. S34-7.
3. Guennoun, R., et al., Progesterone and allopregnanolone in the central nervous system: response to injury and implication for neuroprotection. J Steroid Biochem Mol Biol, 2015. 146: p. 48-61.
4. Hirst, J.J., et al., Neuroactive steroids in pregnancy: key regulatory and protective roles in the foetal brain. J Steroid Biochem Mol Biol, 2014. 139: p. 144-53.
5. Malek, A., Role of IgG antibodies in association with placental function and immunologic diseases in human pregnancy. Expert Rev Clin Immunol, 2013. 9(3): p. 235-49.
6. Svensson-Arvelund, J., et al., The placenta in toxicology. Part II: Systemic and local immune adaptations in pregnancy. Toxicol Pathol, 2014. 42(2): p. 327-38.
7. Gordon, Z., et al., Ex Vivo Human Placental Perfusion Model for Analysis of Fetal Circulation in the Chorionic Plate. J Ultrasound Med, 2016. 35(3): p. 553-60.
Figures