0861
Diffusion tensor imaging and T2 measurements are sensitive to changes in muscle tear due to healing1Leeds Biomedical Research Centre, The University of Leeds, Leeds, United Kingdom, 2Leeds Institute of Cardiovascular and Metabolic Medicine, The University of Leeds, Leeds, United Kingdom, 3Medical Physics and Engineering, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom, 4Leeds Institute of Rheumatic and Musculoskeletal Medicine (LIRMM), The University of Leeds, Leeds, United Kingdom, 5Siemens Healthcare, Erlangen, Germany
Synopsis
The aim of this study was to investigate the ability of diffusion tensor imaging (DTI) and T2 measurements to detect changes due to healing in athletes with muscle tears. 13 professional athletes were imaged within 2 days of injury and at the point that they returned to training. Regions of interest depicting the tear were drawn at visit 1 and were propagated to parameter maps from both visits taking into account motion between images. The study showed significant differences in DTI parameters and T2 values between visits, implying that these measures may be useful quantitative markers in assessing muscle healing.
Introduction
Acute muscle injuries are common in athletes, with tears due to active traumatic events having a high prevalence (1). Despite an increase in imaging based assessments of muscle tears and several proposed grading systems the prevalent MRI-based classification is still based on a qualitative quantification of the amount of torn fibres (2). Diffusion tensor imaging (DTI) using Stimulated Echo Acquisition Mode (STEAM) is particularly suited to muscle imaging as it allows long diffusion times without strong T2-induced SNR loss and improved fat suppression of the olefinic fat peak (3). STEAM-DTI has been used successfully in muscle tear patients to show differences between tear sites and contralateral healthy muscles (4), but has not previously been used to show tissue changes due to healing in a longitudinal study design. The aim of this study was to demonstrate quantitative changes in STEAM-DTI and T2-measurements in muscle tears over time.Methods
13 professional athletes were included in this NREC ethically approved longitudinal pilot study. Participants were imaged on a MAGNETOM Verio 3T MR system (Siemens Healthcare, Erlangen, Germany) within 2 days of muscle tear in the thigh or calf. A second scan was performed when the participant was determined “fit to return to training” by the team physiotherapist (range 12-56 days post injury). Imaging consisted of a T1-weighted STIR volume positioned using an anatomical reference point (the insertion point of the rectus femoris into the tendon). The slice best depicting the muscle tear was identified for quantitative imaging, which consisted of T2 measurements made using a turbo spin echo (TSE) sequence and STEAM-DTI. The STEAM prototype sequence, with an echo planar imaging (EPI) readout, used spectral attenuated inversion recovery (SPAIR) fat suppression, TR/TE: 6300ms/42.4ms, slice thickness 5mm, matrix 128x128, nominal b-values of 0 and 500 mm2s-1, 6 diffusion directions, an echo spacing of 0.76ms and a long diffusion mixing time of 980ms to maximise sensitivity to restricted diffusion. Mean diffusivity (MD) and fractional anisotropy (FA) parameter maps were generated. The TSE sequence used TR=1500ms, TE=9.9ms to 153.4ms (16 echoes, equally spaced) and SPAIR fat suppression. An experienced radiologist drew regions of interest (ROIs) within the tear site, haematoma (if present), oedema, and nearby normal muscle on the visit 1 images. These ROIs were propagated on to the visit 2 images using image registration to correct for movement (figure 1). To correct for misalignment between visits the visit 2 T1-weighted image was registered to the corresponding visit 1 image using an intensity-based affine registration with normalized mutual information as the similarity metric. The image transform from this step was then applied to the individual visit 2 TSE images and diffusion maps. Furthermore, to correct for movement between images in the same visit, a rigid image registration was applied between the T1-weighted image and the TSE and diffusion maps. To obtain T2 estimates a mono-exponential T2-fit was applied to mean signal intensities from ROIs at each echo time taken from the TSE image series. A paired samples t-test was used to test for differences in quantitative parameters between visits for each ROI using a significance level of 0.05.Results
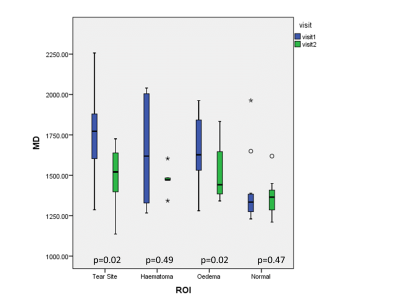
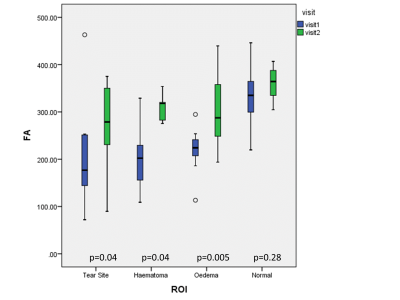
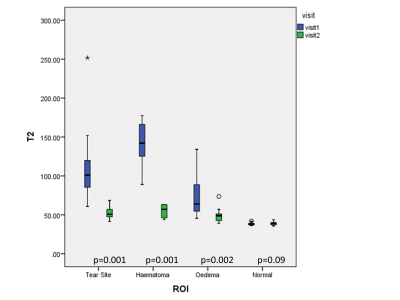
The radiologist’s qualitative, visual assessment of registration performance was good, and no manual corrections were necessary. MD was significantly reduced at visit 2 in the tear site and oedema but not in haematoma and normal muscle (figure 2). FA increased significantly in the later scan in all tear ROIs (figure 3) whereas T2 was decreased in the later scans (figure 4). There were no differences in T2 or diffusion parameters in healthy tissue between visits.Discussion
The reduction in MD with healing is consistent with reduced fluid content and/or increased muscle fibre order, as is the observed increase in FA. The reduction in T2 with healing is also consistent with a reduced fluid content and was the strongest effect observed, implying that T2 measurements were the most sensitive to change in this study. There were no significant differences in the normal muscle between visits as expected. These results show that both DTI and T2 measurements are sensitive to changes due to tear healing. This is likely to be due to changes in fluid content or muscle fibre structure as well as changes in the volume of the tear site. These findings provide evidence that such measures show potential as quantitative tear severity scores.Conclusion
T2 measurements and STEAM DTI measurements are sensitive to changes in muscle tear, haematoma and oedema due to healing.Acknowledgements
This paper presents independent research funded by the National Institute for Health Research (NIHR) and Health Education England. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. We are grateful to Rob Evans and Brian Chaka for carrying out the MR studies.References
1. Lee JC, Mitchell AWM, Healy JC. Imaging of muscle injury in the elite athlete. Br J Radiol. 2012;85(1016):1173–85.
2. Hamilton B, Valle X, Rodas G, Til L, Grive RP, Rincon JAG, et al. Classification and grading of muscle injuries: A narrative review. Br J Sports Med. 2015;49(5):306.
3. Karampinos DC, Banerjee S, King KF, Link TM, Majumdar S. Considerations in high resolution skeletal muscle DTI using single-shot EPI with stimulated echo preparation and SENSE. NMR Biomed. 2008;6(9):2166–71.
4. Giraudo C, Motyka S, Weber M, Karner M, Resinger C, Feiweier T, et al. Normalized STEAM-based diffusion tensor imaging provides a robust assessment of muscle tears in football players : preliminary results of a new approach to evaluate muscle injuries. Eur Radiol. European Radiology; 2018;
Figures