0772
Toward high-SNR, motion-robust diffusion MRI of the liver using optimized gradient waveforms, non-gated free-breathing acquisitions, and motion-corrected averaging1Radiology, University of Wisconsin, Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin, Madison, Madison, WI, United States, 3Biomedical Engineering, Vanderbilt University, Nashville, TN, United States, 4Institute of Imaging Science, Vanderbilt University, Nashville, TN, United States
Synopsis
Liver DWI suffers from signal voids introduced by elastic motion, mis-registration due to respiratory motion and low SNR. We propose to develop and evaluate a novel free-breathing DWI technique appropriate for the abdomen, in order to provide high SNR efficiency with predictable scan times, while avoiding motion-related artifacts. Evaluations showed that compared to respiratory-triggering acquisitions, the proposed DWI technique provided higher SNR and predictable scan times. Further, a motion-corrected averaging algorithm has the potential to correct for motion-related artifacts. Using optimized gradient waveforms, non-gated free-breathing acquisitions, and motion-corrected averaging techniques, high-SNR and motion-robust DWI of the liver may be achieved.
Introduction
Diffusion-weighted imaging (DWI) in the abdomen has multiple clinical applications, including the detection, characterization, and treatment monitoring of cancer12. However, liver DWI faces several major challenges including signal voids introduced by elastic motion, mis-registration due to respiratory motion and low SNR3. Recent works have developed optimized diffusion waveforms that enable motion-robust liver DWI456. Nevertheless, motion-robust DWI typically requires longer TEs, which leads to a loss of SNR4. Multi-repetition acquisitions with respiratory triggering (RT) are able to enhance SNR and co-localization7. However, RT lengthens the repetition time (TR) and leads to unpredictable scan time due to variability in patients’ breathing patterns8. Therefore, the purpose of this work is to develop and evaluate a novel free-breathing (FB) DWI technique in order to provide high SNR with predictable scan times, while avoiding motion-related artifacts. The technique combines motion-robust diffusion waveforms, high SNR from non-gated FB acquisitions, and motion-corrected averaging using a non-local means algorithm (NLM).Methods
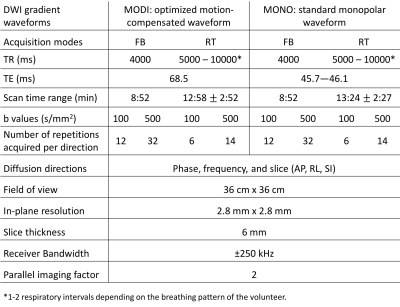
A motion-robust M1-optimized diffusion gradient waveform (MODI) and a standard monopolar waveform (MONO) were used to acquire DWI of the liver. For each gradient waveform, both FB and RT acquisitions were performed. For the FB acquisitions, an NLM-based algorithm (Fig.1) was used to address motion across repetitions and diffusion directions for each b value. After IRB approval and informed written consent, six healthy volunteers were scanned at 3T (GE Signa Premier) using flexible receive coils (AIR Technology, GE Healthcare, Waukesha, WI). The acquisition parameters are shown in Table.1. Three technical components were assessed: diffusion waveform (MODI vs. MONO); respiratory-motion mitigation (RT vs. FB); and signal averaging (direct averaging vs. NLM). For each acquisition and signal averaging method, DW images and corresponding ADC maps were generated. Performance comparisons included: ADC measurements in right and left liver lobes in MODI vs. MONO, SNR of averaged FB vs. RT images under comparable scan times, and motion-robustness and SNR of direct averaging (DA) vs. NLM. Additionally, assessment of respiratory-motion mitigation and signal averaging methods was performed retrospectively using fewer repetitions (50% and 20%), in order to assess the potential for faster acquisitions with the proposed approach. For each choice of technical components and number of repetitions, signal and noise levels of ADC maps were estimated by calculating means and standard deviations over co-localized ROIs.
Results
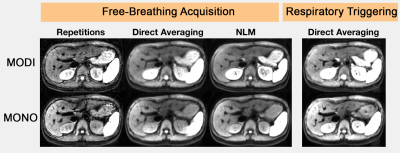
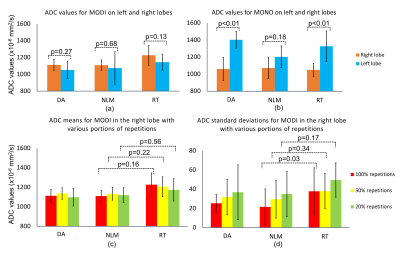
Diffusion waveform (MODI vs. MONO): ADC values are more homogeneous across left and right lobes on MODI than on MONO (Fig.2,3). Regardless of acquisition modes and signal-averaging methods, ADC comparison between left and right lobes showed no significant difference in MODI (Fig.4.a). In contrast, a significant difference was observed in MONO (Fig.4.b), unless NLM was applied.
Respiratory-motion mitigation (RT vs. FB): Scan times with FB for both waveforms were fixed across volunteers, while RT scan times were longer on average and varied substantially across volunteers (Table.1). FB data reconstructed with NLM had similar signal levels but significantly lower noise levels compared to RT on MODI when 100% repetitions were used (Fig.4.c,d). As number of repetitions decreased, NLM tended to maintain lower noise levels than RT (Fig.3).
Signal averaging (DA vs. NLM): In both DWI and ADC maps (Fig.2,3), compared to DA, NLM reduced the mis-registration due to body motion, showed increased homogeneity throughout the liver, and higher spatial resolution overall. The mean and standard deviations of ADC values of NLM were comparable to those of DA; no significant difference found between them for any choice of waveforms or number of repetitions in either lobe (Fig.4).
Discussion
The proposed technique combines motion-robust gradient waveforms (MODI) with FB acquisitions and motion-corrected averaging in order to enable abdominal DWI without motion artifacts and with high SNR. Compared to standard RT acquisitions, the proposed DWI technique provides higher SNR and predictable scan times even in the presence of irregular breathing patterns (which lead to scan-time variability in RT imaging). The proposed NLM algorithm has the potential to correct for motion across repetitions, diffusion directions, and b values. However, this study has several limitations. Further optimization and characterization of proposed technique are desirable. Indeed, NLM includes a number of tunable parameters that may be optimized, depending on the degree of respiratory motion and underlying SNR. Additionally, validation in a larger patient cohort is required and will be included in future work. Nevertheless, the proposed method shows the potential to improve workflow (i.e., predictable and shortened scan times) and image quality (i.e., motion robustness and improved SNR) compared to current methods for abdominal DWI.Conclusion
Using optimized gradient waveforms, non-gated free-breathing acquisitions, and motion-corrected averaging techniques, high-SNR and motion-robust DWI of the liver may be achieved.Acknowledgements
The authors would like to acknowledge research support from GE Healthcare.References
[1] Koh, Dow-Mu, and David J. Collins. "Diffusion-weighted MRI in the body: applications and challenges in oncology." American Journal of Roentgenology 188, no. 6 (2007): 1622-1635.
[2] Gourtsoyianni, Sofia, Nickolas Papanikolaou, Spyros Yarmenitis, Thomas Maris, Apostolos Karantanas, and Nicholas Gourtsoyiannis. "Respiratory gated diffusion-weighted imaging of the liver: value of apparent diffusion coefficient measurements in the differentiation between most commonly encountered benign and malignant focal liver lesions." European Radiology 18, no. 3 (2008): 486-492.
[3] Kim, Tonsok, Takamichi Murakami, Satoru Takahashi, Masatoshi Hori, Kyo Tsuda, and Hironobu Nakamura. "Diffusion-weighted single-shot echoplanar MR imaging for liver disease." AJR. American Journal of Roentgenology 173, no. 2 (1999): 393-398.
[4] Zhang, Yuxin, Jim Holmes, Diego Hernando. "Motion-Robust and Blood-Suppressed M1-Optimized Diffusion MR Imaging of the Liver. " Magnetic Resonance in Medicine. Submitted for review.
[5] Pena-Nogales, Oscar, Yuxin Zhang, Xiaoke Wang, Rodrigo Luis-Garcia, Santiago Aja-Fernández, James H Holmes, and Diego Hernando. "Optimized Diffusion-Weighting Gradient Waveform Design (ODGD) formulation for motion compensation and concomitant gradient nulling." (2018). Magnetic Resonance in Medicine (2018). Early view.
[6] Aliotta, Eric, Holden H. Wu, and Daniel B. Ennis. "Convex optimized diffusion encoding (CODE) gradient waveforms for minimum echo time and bulk motion–compensated diffusion‐weighted MRI." Magnetic Resonance in Medicine 77, no. 2 (2017): 717-729.
[7] Kandpal, Harsh, Raju Sharma, Kulwant Singh Madhusudhan, and Kulwant Singh Kapoor. "Respiratory-triggered versus breath-hold diffusion-weighted MRI of liver lesions: comparison of image quality and apparent diffusion coefficient values." American Journal of Roentgenology 192, no. 4 (2009): 915-922.
[8] Kwee, Thomas C., Taro Takahara, Dow‐Mu Koh, Rutger AJ Nievelstein, and Peter R. Luijten. "Comparison and reproducibility of ADC measurements in breathhold, respiratory triggered, and free‐breathing diffusion‐weighted MR imaging of the liver." Journal of Magnetic Resonance Imaging: An Official Journal of the International Society for Magnetic Resonance in Medicine 28, no. 5 (2008): 1141-1148.
Figures